Atlas of Hematopathology
Morphology, Immunophenotype, Cytogenetics, and Molecular Approaches
- 756 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Atlas of Hematopathology
Morphology, Immunophenotype, Cytogenetics, and Molecular Approaches
About This Book
As the definitive diagnostic atlas of the diseases of the hematopoietic system, the Atlas of Hematopathology appeals to a wide range of people who are being trained in a variety of medical fields or practicing as non-hematopathologists, and therefore, are looking for a book which can provide information in a clear, focused format, with no excessive text or details. The atlas offers effective guidance in evaluating specimens from the lymph nodes, bone marrow, spleen, and peripheral blood, enabling clinicians to deliver more accurate and actionable pathology reports. Practicing physicians and those in pathology and hematology training also gain a better understanding of the nature of hematologic disorders and improve their diagnostic skills along the way. Taking a unique multi-disciplinary approach, the book covers conventional histopathology and cytopathology, as well as all important complementary diagnostic tests, such as immunophenotyping (immunohistochemical stains and flow cytometry), karyotyping, FISH and DNA/molecular studies. It offers concise textual and extensive visual coverage of both neoplastic and non-neoplastic hematology disorders, with the neoplastic hematology sections presented according to the most recent WHO classifications. There is also an introduction to the normal structures of hematopoietic tissues and the various multidisciplinary techniques. The atlas contains more than 900 high-quality color images that mirror the findings that fellows and clinicians encounter in practice. It provides information in a quick, simple and user-friendly manner, attracting those who are in training or are not considered experts in the field. Residents, fellows, practicing clinicians, and researchers in pathology, hematology, hematology/oncology, as well as graduate students in pathology and other clinicians workings in clinical hematology laboratories will all find it useful.
- Saves clinicians and researchers time in quickly accessing the very latest details on the diverse clinical and scientific aspects of hematopathology, as opposed to searching through thousands of journal articles
- For clinicians, fellows, and residents, correct diagnosis (and therefore correct treatment) of diseases depends on a strong understanding of the molecular basis for the disease – hematologists, pathologists, oncologists, and other clinicians will benefit from this clear, focused, annotated format
- Companion web site features over 900 images from the book!
Frequently asked questions
Information
1
Structure and Function of Hematopoietic Tissues
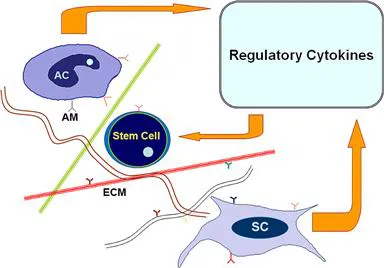
| Type | Comments |
| Collagen (reticulin) | Consisting of various subtypes. Erythroid and myeloid precursors adhere to collagen types I and VI |
| Fibronectin | Attaches to early erythroid precursors and other hematopoietic and stromal cells |
| Hemonectin | Myeloid precursors adhere to laminin. Regulates leukocyte chemotaxis. |
| Proteoglycans | Components containing heparin sulfate, chondritin sulfate, and hyaluronic acid. Interact with laminin and type IV collagen and play a role in cytokine presentation and cell differentiation |
| Thrombospondin | Interacts with collagen, fibronectin, and CD36 |
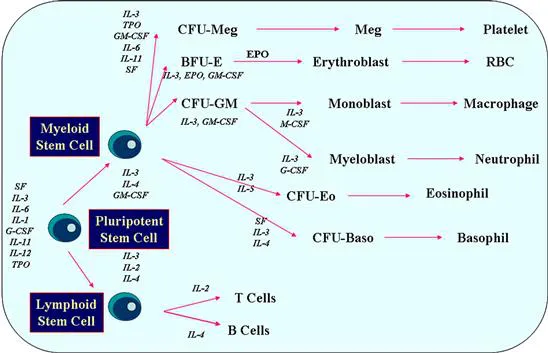
| Cytokine | Primary Effect |
| GM-CSF1 | Granulocyte and macrophage colony formation, functional enhancement of mature forms |
| G-CSF2 | Granulocyte colony formation, functional enhancement of granulocytes |
| M-CSF (CSF-1)3 | Macrophage colony formation, functional enhancement of monocytes and macrophages |
| Erythropoietin (EPO) | Erythropoiesis, possible enhancement of megakaryocyte proliferation |
| Thrombopoietin (TPO) | Megakaryocyte proliferation, platelet production |
| Steel factor (c-kit ligand) | Stem cell and mast cell proliferation |
| Interleukin (IL)-1 | Promoter of hematopoiesis, inducer of other factors, B- and T-cell regulator, endogenous pyogen |
| IL-2 | T-cell growth factor, may inhibit G/M colony formation and erythropoiesis |
| IL-3 (Multi-CSF) | G/M colony formation, syngeneic effects on EPO, eosinophil, mast cell, and megakaryocyte colony formation |
| IL-4 | B-cell proliferation, IgE production |
| IL-5 | Eosinophil growth and B-cell differentiation |
| IL-6 | B-cell differentiation, synergistic effects on IL-1 |
| IL-7 | Development of B and T cell precursors |
| IL-8 | Granulocyte chemotactic factor |
| IL-9 | Growth of mast cells and T cells |
| IL-10 | Inhibitor of inflammatory and immune responses |
| IL-11 | Synergistic effects on growth of stem cells and megakaryocytes |
| IL-12 | Promoter of Th1 and suppressor of Th2 functions |
| IL-13 | B-cell proliferation, IgE production |
| IL-14 | High molecular weight B-cell growth factor |
| IL-15 | Activates T cells, neutrophils and macrophages |
| IL-16 | Chemotactic factor for helper T cells |
| IL-17 | Promotes T cell proliferation, pro-inflammatory activities |
| IL-18 | Activates T cells, neutrophils, and fibroblasts |
| IL-19 | Member of IL-10 family; transcriptional activator of IL-10 |
| IL-20 | Member of IL-10 family with epidermal function |
| IL-21 | Improves proliferation of T cells and B cells, and enhances natural killer (NK) cytotoxic activities |
| IL-22 | Member of IL-10 family; induces inflammatory responses |
| IL-23 | Activates autoimmune responses |
| IL-24 | Member of IL-10 family; tumor suppressor molecule |
| IL-25 | Capable of amplifying allergic inflammation |
| IL-26 | Member of IL-10 family; plays a role in mucosal and cutaneous immunity |
| TGF4-β | Suppresses BFU-E, CFU-S, and HPP-CFC |
| Interferons | Suppress BFU-E, CFU-GEMM, and CFU-GM |
| TNF5-α and -β | Suppress BFU-E, CFU-GEMM, and CFU-GM |
| PGE6-1 and -2 | Suppress GFU-GM, GFU-G, and GFU-M |
| Lactoferrin | Suppresses release of IL-1 |
Table of contents
- Cover image
- Title page
- Table of Contents
- Copyright
- Preface
- Acknowledgments
- 1. Structure and Function of Hematopoietic Tissues
- 2. Principles of Immunophenotyping
- 3. Principles of Cytogenetics
- 4. Principles of Molecular Techniques
- 5. Morphology of Abnormal Bone Marrow
- 6. Reactive Lymphadenopathies
- 7. Bone Marrow Aplasia
- 8. Myelodysplastic Syndromes/Neoplasms—Overview
- 9. Myelodysplastic Syndromes/Neoplasms—Classification
- 10. Myeloproliferative Neoplasms—Overview
- 11. Chronic Myelogenous Leukemia
- 12. Myeloproliferative Neoplasms Associated with JAK2 Mutation
- 13. Chronic Neutrophilic and Chronic Eosinophilic Leukemias
- 14. Mastocytosis
- 15. Myelodysplastic/Myeloproliferative Neoplasms
- 16. Hematologic Neoplasms Associated with Eosinophilia and PDGFRA, PDGFRB, or FGFR1 Rearrangement
- 17. Acute Myeloid Leukemia—Overview
- 18. Acute Myeloid Leukemias with Recurrent Genetic Abnormalities
- 19. Acute Myeloid Leukemia with Myelodysplasia-Related Changes
- 20. Therapy-Related Myeloid Neoplasms
- 21. Acute Myeloid Leukemia, Not Otherwise Specified
- 22. Myeloid Proliferations Related to Down Syndrome
- 23. Lymphoblastic Neoplasms—B-Lymphoblastic Leukemia/Lymphoma
- 24. Lymphoblastic Neoplasms—T-Lymphoblastic Leukemia/Lymphoma
- 25. Acute Leukemias of Ambiguous Lineage
- 26. Mature B-Cell Neoplasms—Overview
- 27. Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma
- 28. B-Cell Prolymphocytic Leukemia
- 29. Lymphoplasmacytic Lymphoma/Waldenström’s Macroglobulinemia
- 30. Hairy Cell Leukemia
- 31. Splenic Marginal Zone Lymphoma
- 32. Nodal Marginal Zone Lymphoma
- 33. Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT Lymphoma)
- 34. Follicular Lymphoma
- 35. Mantle Cell Lymphoma
- 36. Diffuse Large B-Cell Lymphoma
- 37. Diffuse Large B-Cell Lymphoma Subtypes
- 38. Other Lymphomas of Large B Cells
- 39. Burkitt Lymphoma
- 40. Primary Cutaneous B-Cell Lymphomas
- 41. Plasma Cell Neoplasms
- 42. Mature T- and NK-Cell Neoplasms—Overview
- 43. Large Granular Lymphocytic Neoplasms and Related Disorders
- 44. T-Cell Prolymphocytic Leukemia
- 45. Adult T-Cell Leukemia/Lymphoma
- 46. Hepatosplenic T-Cell Lymphoma
- 47. Enteropathy-Associated T-Cell Lymphoma
- 48. Mycosis Fungoides and Sézary Syndrome
- 49. Other Primary Cutaneous T-Cell Lymphoproliferative Disorders
- 50. Angioimmunoblastic T-Cell Lymphoma
- 51. Anaplastic Large Cell Lymphomas
- 52. Peripheral T-Cell Lymphoma, Not Otherwise Specified
- 53. Nodular Lymphocyte Predominant Hodgkin Lymphoma
- 54. Classical Hodgkin Lymphoma
- 55. Immunodeficiency Disorders
- 56. Iatrogenic Immunodeficiency-Associated Lymphoproliferative Disorders
- 57. Lymphocytopenia and Lymphocytosis
- 58. Histiocytic Disorders
- 59. Disorders of Dendritic Cells
- 60. Granulocytic Disorders
- 61. Disorders of Red Blood Cells—Anemias
- 62. Disorders of Megakaryocytes and Platelets
- 63. Post-Therapy Changes
- Index