![]()
Chapter 1
Introduction
Regenerative Medicine and Solid Organ Transplantation from a Historical Perspective
Joseph P. Vacantia, Jean-Bernard Otteb and Jason A. Wertheimc, aLaboratory of Tissue Engineering and Organ Fabrication, Massachusetts General Hospital, Boston, MA, bUniversité Catholique de Louvain, Cliniques Saint-Luc, Brussels, Belgium, cComprehensive Transplant Center, Department of Surgery, Northwestern University Feinberg School of Medicine, Institute for BioNanotechnology in Medicine and Chemistry of Life Processes Institute, Northwestern University, Chicago, IL
Regenerative medicine and transplantation are rooted in distinct but major scientific advancements during the last 15 and 50 years, respectively. To introduce this text, we review the major milestones that led to the development of solid organ transplantation and regenerative medicine. The success of transplantation has led to the need for regenerative medicine. The number of patients waiting for an organ for transplantation has surpassed 117,000. Many of these candidates may not receive an organ due to the limited supply of cadaveric grafts or those donated by altruistic living donors. It is the shared hope that regenerative medicine may one day augment organ transplantation by developing a new source of organs or potentially rehabilitating those that are not transplantable. This chapter summarizes major advancements in both fields including vascular reconstruction, organ preservation, immunosuppression, operational tolerance, novel stem cell sources, biodegradable scaffolds, and new methods to develop vascularized organ units.
Keywords
Organ shortage; Regenerative medicine; Solid organ transplantation
Chapter Outline
1.1 Introduction
1.2 Major Advances in Organ Transplantation
1.2.1 Vascular Reconstruction
1.2.2 Organ Preservation
1.2.3 Artificial Support
1.2.4 Immunosuppression
1.2.5 Operational Tolerance
1.2.6 Organ Recovery and Definition of Brain Death
1.2.7 Living Donation
1.2.8 HLA Typing and Crossmatch
1.3 Regenerative Medicine
1.3.1 A New Term in Transplantation: Regenerative Medicine
1.3.2 Characteristics of Regenerative Tissues
1.3.3 Polymer Development
1.3.4 Early Tissue Development
1.3.5 Cell Source
1.3.6 Soft Tissue Regeneration as Applied to Battlefield Medicine
1.3.7 Planar Acellular Dermal Matrices
1.3.8 Vascularization of Tissue-Engineered Organs
1.3.9 Perfusion Decellularization, Using Nature’s Vascular Network
1.3.10 Specific Organ Transplantation History and Link to Engineering
1.3.11 Concluding Remarks
References
1.1 Introduction
As a therapeutic modality, solid organ transplantation has been available to patients in need for the past half-century, however, it is only within the past 30 years that the development of immunosuppression has allowed for long-term graft survival with minimal risk of rejection. The history of organ transplantation is a remarkable journey of scientific experimentation, progress and failures, miraculous discoveries, and personal sacrifice on the part of those early donors and recipients of transplanted organs. The first modern-day studies in transplantation began at the turn of the twentieth century in which skin grafting between animals initiated the first series of experiments that eventually led to a scientific understanding of graft rejection. This, in turn, opened the door to the modern era of human transplantation with the first successful kidney transplant between two identical siblings in 1954 by Joseph Murray at the Peter Bent Brigham Hospital in Boston. Since that time, advances in immunosuppression, development of complex operative techniques, and patient/donor selection have made organ transplantation a successful clinical modality that touches tens of thousands of patients worldwide every year.
Regenerative medicine, on the other hand, is a relatively newer concept in medical care that builds upon the principles of stem cell technology and regrowth of organs and tissues to provide new treatments to old ailments. The ability of the body to regenerate, or regrow, itself is first evident in nature. Salamanders have the ability to regrow their tails [1]. Sea cucumbers, if divided into pieces, become new, individual entities. Some spiders regrow legs, starfish can regenerate new arms. Perhaps an early interpretation of regenerative medicine may have been embodied in the concept of the “fountain of youth.” Herodotus, an ancient Greek historian born in the fifth century BC first described a special liquid that gave the people of Ethiopia longevity. In the sixteenth century, the conquistador Juan Ponce de León explored the newly discovered Americas and was charged with finding the fountain of youth. However, these historical interpretations of magical water restoring youth are not entirely in line with the modern-day concept of “regenerative medicine.” Perhaps the most accurate, modern-day definition is that of Leland Kaiser who wrote in 1992 that regenerative medicine “attempts to change the course of chronic disease” to restore normal function to tissues, cells, and organs [2]. This concept was later promoted by William Haseltine of Human Genome Sciences (Rockville, MD).
The earliest references to organ transplantation and regeneration are embodied in the Chimera and the Hydra in ancient Greek mythology. The Chimera was first introduced in Homer’s the Odyssey as a collection of different body parts taken from a goat, lion, and dragon. The Hydra was a multiheaded monster that was thought impossible to defeat because once severed, a new head regrew in its place. Hercules eventually defeated the Hydra by burning its neck before a new head grew back as part of his 12 Labors.
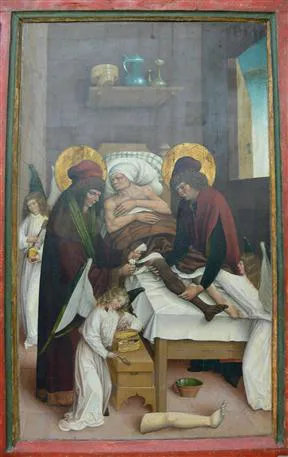
Ancient Chinese texts documented the first human-to-human transplant and recount the exchange of two hearts between soldiers by surgeon Tsin Yue-Jen. This is reportedly the first known description of body to body transplantation [3]. In the third century AD, Christian mythology described the first cadaveric transplant when Saints Damien and Cosmas transplanted a cadaver leg onto a soldier (Figure 1.1). The first report in a medical journal describing a human-to-human skin transplant first appeared in 1881. The recipient was burned while leaning against a metal door during a lightning strike.
Figure 1.1 In the third century AD, Christian mythology described the first cadaveric transplant when Saints Damien and Cosmas transplanted a cadaver leg onto a soldier. Legendary transplantation of a leg by Saints Cosmas and Damian, assisted by Angels (Württembergisches Landesmuseum Stuttgart), available at: http://en.wikipedia.org/wiki/File:Beinwunder_Cosmas_und_Damian.webp.
Transplantation and regenerative medicine perhaps both have their most significant, early contributions to skin grafting, and soft tissue reconstruction. Sir Harold Giles was the first surgeon to take skin from a healthy portion of the body and transfer it onto a burned segment. This was the case of British soldier Walter Yeo who sustained deep facial burns around his eyelids and eyes while maintaining guns aboard the British ship HMS Worspite in 1916. As medicine progressed throughout the early twentieth century, vascular bypass was established as a means to circumvent blocked arteries in the heart, abdomen, and lower extremity. It is commonly known that the body’s own vascular conduits in the form of small arteries and veins perform much better when taken from their original location and used as a bypass conduit compared to synthetically constructed, inert bypass grafts. The development of new vascular channels is another important component of regenerative medicine and shares common themes with transplantation. In 1960 at Albert Einstein College of Medicine–Bronx Municipal Hospital Center, Robert Goetz and his team performed the first coronary artery bypass surgery in 1960. Three years later, Thomas Starzl performed the first human liver transplantation in 1963. And, in the 50 years that have postdated that achievement, organ transplantation has expanded throughout the United States and the world due to revolutionary advancements in immunosuppression, surgical technique, and patient/donor selection. Now, over 117,000 patients are waiting for an organ for transplantation in the United States alone and this increasing trend has never been reversed. The promise of organ transplantation in the regenerative medicine era is the hope that one day organs and tissues can be developed “on demand” to supply all patients in need of organ and tissue replacement.
1.2 Major Advances in Organ Transplantation
1.2.1 Vascular Reconstruction
Every solid organ transplant requires precise vascular reconstruction. The technique of triangular vascular anastomosis was devised by Alexis Carrel at the turn of the twentieth century at the University of Lyon and further refined with Charles Claude Guthrie at the University of Chicago. This technique was used by Carrel to develop renal transplantation. The Noble Prize in Physiology was awarded in 1912 to Carrel for this pioneering work.
1.2.2 Organ Preservation
Carrel and Charles Lindbergh pioneered ex vivo pulsatile organ perfusion at the Rockefeller Institute in the 1930s. In 1964, Lillehei et al. published an early paper about in vitro preservation of the kidney and the heart by a combination of hypothermia and hyperbaric oxygenation [4].
Dr Francis O. Belzer developed ex vivo renal preservation by perfusion of recovered kidneys with cryoprecipitated plasma allowing preservation of dog kidneys for up to 72 h and successful renal human transplantation after 17 h of storage [5]. Later, he developed a miniature portable perfusion machine, the precursor of the device that is now used worldwide to pump kidneys with cold perfusate.
The first solution allowing cold organ preservation after initial perfusion was formulated by Collins et al. [6]. Although the duration of preservation of the kidney and liver was somewhat limited, Collins’ solution was used for nearly 20 years.
The University of Wisconsin (UW) solution developed by Belzer et al. permitted the extension of the duration of cold storage. It has revolutionized cold storage of the liver and the pancreas [7].
1.2.3 Artificial Support
Patients with chronic renal disease need extracorporeal dialysis while waiting for a donated kidney. The artificial kidney was devised by the Dutch physician Willem Johan Kolff in 1943, under the Nazis’ occupation of the Netherlands. The first patient with acute renal failure was saved by Willem Kolff in 1945. He continued his research on renal dialysis at the Mount Sinai Hospital which was granted one of the first five machines built by Kolff [8].
After his move to the University of Utah, Kolff devised the first artificial heart that was named after a coworker, Robert Jarvis. This research paved the way for artificial cardiac support to become a bridge to definitive heart transplantation for patients awaiting a transplant, either acutely with extracorporeal circulation with ECMO or chronically with an implantable left ventricular assist device.
Renal replacement in the form of hemodialysis requires access to an artery and a vein. The remarkable achievement of Belding Scribner at the University of Washington was to develop an original arterial-venous shunt made of Teflon that was used worldwide for hemodialysis access in patients with end-stage renal disease for decades prior to the introduction of the arterial-venous fistula [9].
1.2.4 Immunosuppression
The first attempts at immunosuppression included total body irradiation and steroids but were eventually unsuccessful. Pharmacological immunosuppression became the standard of care with the development ...