1.1 Introduction
Advances in cardiovascular procedures would have not been possible without the concomitant developments in biotechnology. The application of biomaterials spans from prosthetic heart valves, ventricular assist devices, cardiac pacemakers and endovascular implants, to suture material and bio-adhesives. Materials and devices used for the restoration of anatomical and physiological circulatory properties are not without associated risks and potential complication, both in the immediate as well as the long-term period, following implantation within the recipient.
Implant building blocks vary from an array of metals and their alloys, polymers and ceramics. Naturally occurring materials such as collagen, hyaluronan and dextran are commonly used. Synthetic polymers used for the construction of implantable devices include polylactic acid, polylactic-co-glycolic acid, polyvinyl alcohol and others (Onuki et al., 2008). The majority of implanted devices are composed of more than one type of material and are referred to as complex composition implants. Although these materials have been used extensively with good functional results, there are issues of biocompatibility. The need to surpass physical limitations and improve the biomechanical profile of metals has led to the development of novel metal alloys. In addition to superior physical and chemical properties regarding strength, durability and resistance to corrosion, certain alloys have very unique properties. An example is nickel-titanium (nitinol) alloys that exhibit shape memory and superelasticity, making it one of the most widely used materials in medical prostheses.
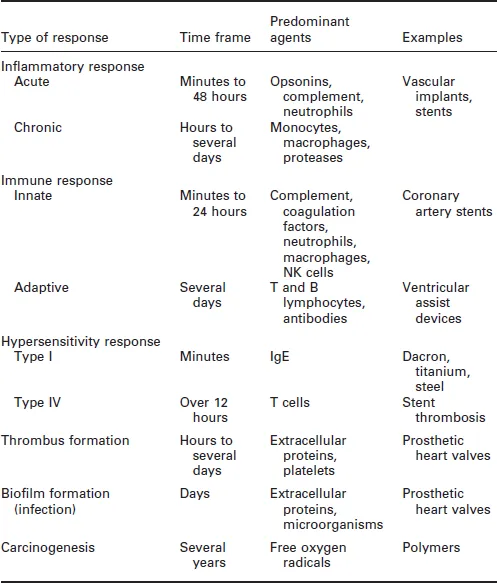
The tissue response to implanted materials is a complex process. It entails a variety of pathways that may include the generation and activation of interacting humoral and molecular components. These processes may be acute, taking place over minutes, or long term, spanning many years (Table 1.1). This chapter aims to present the commonest types of tissue response to materials used for the construction of implantable medical devices. It describes processes such as inflammation, immune response, hypersensitivity, formation of thrombus or biofilm and carcinogenesis. Each section contains a description of the molecular and cellular pathways involved in these processes.
Table 1.1
Commonest types of tissue response to implanted materials
1.2 Inflammatory response
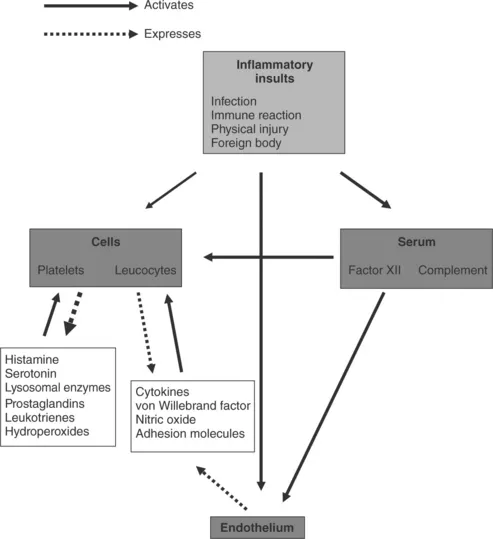
Inflammation is the initial, non-specific response of vascularised tissue to a variety of injuries. It represents the attempt of the body to eliminate the injuring agent. Our knowledge of the complicated network of molecules that interconnects different inflammatory pathways during cardiac surgery started to expand at a later time following advances in basic sciences. The inflammatory response may be local or systemic. Although inflammation aims to exercise a healing effect against injury, the immune system may erroneously attack body tissues at a larger scale than necessary. The inflammation process comprises primarily activation of serum molecular cascades and responses of endothelium and leucocytes. It may be triggered by stimuli such as infection, immune reaction, physical injury or foreign bodies (Rock and Kono, 2008). Figure 1.1 illustrates mediators participating in acute inflammatory response.
1.1 Mediators participating in the acute systemic inflammatory response.
Implantable materials are perceived as foreign bodies and elicit inflammatory response through injury to local tissues, which prompts the host to repair the damage. The immediate injury results in activation of endothelial cells and increased interaction with activated neutrophils. This process results in damage of endothelial integrity, increased endothelial permeability and tissue oedema. There is also activation of the coagulation cascade and components of the immune system. The products of these responses collectively form a provisional matrix consisting of fibrin, activated platelets, inflammatory cells and endothelial cells. The provisional matrix acts as a site for cell adhesion and provides activating and inhibiting substances to facilitate proliferation within the lesion. The process is well established and clearly illustrated in coronary stent insertion where the immediate injury is to vascular endothelium caused by stent strut penetration (Edelman and Rogers, 1998). The inflammatory response is a part of normal healing. However, abnormal proliferation of cells and formation of an extracellular matrix may result in intimal hyperplasia (Farb et al., 2004), which can cause significant stenosis and subsequent morbidity. A similar process is recognised at anastomotic sites in vascular bypass grafts (Glagov et al., 1991). One realises the importance of this fact as significant efforts have been made to design and produce anastomotic devices facilitating construction of coronary graft anastomoses (Falk et al., 2005; Gummert et al., 2007).
The inflammatory response consists of an acute and a chronic phase and is mediated by a vast array of chemicals released from the injured tissue, plasma and cells. These include vasoactive agents, plasma proteases (kinins,complement and coagulation systems), leukotrienes, lysosomal proteases, oxygen-derived free radicals, platelet activating factors, cytokines and growth factors (Anderson, 2004).
Acute inflammation lasts from minutes to 24 to 48 hours. It is characterised by changes in vascular calibre and endothelial permeability. The predominant cell type involved at this stage is the neutrophil, which migrates and binds to the site of injury via chemotactic agents and adhesion molecules respectively. This process results in extravasation of fluid and proteins causing oedema. Opsonins, especially IgG and C3b, promote the recognition and attachment of neutrophils to the surface of a device and may play a role in their activation and subsequent phagocytosis. However, normal phagocytosis does not occur due to the large molecules that tend to make up device materials. Instead leucocytes simply release chemicals in an attempt to degrade the device.
Chronic inflammation may occur naturally in response to prosthetic implants and may persist over long periods due to the continual presence of foreign material. It may follow acute inflammation. Furthermore, displacement or infection of a device are additional stimuli that promote a chronic inflammatory process. This is characterised by the presence of monocytes, macrophages and lymphocytes and proliferation of blood vessels and connective tissue. Monocytes and macrophages, along with cell types from various other tissues in the body, form the reticuloendothelial system. Macrophages are the most important cell in chronic inflammation as they release a variety of products that are involved in the tissue response to prosthetic implants and wound healing such as neutral proteases, chemotactic factors, arachidonic acid metabolites, reactive oxygen metabolites, complement components, coagulation factors, growth-promoting factors and cytokines (Anderson, 2004).
Granulation tissue, the hallmark of wound healing, can be seen as early as 3 to 5 days after device implantation. It is characterised by neovascularisation and proliferation of fibroblasts, which produce proteoglycans and collagen to form a fibrous capsule. Macrophages are also almost always present in granulation tissue. The extent of granulation tissue formation depends on the extent of tissue injury and the area of the defect, caused by injury that must be filled. The foreign-body reaction includes granulation tissue and foreign-body giant cell (FBGC) formation to varying degrees depending on an implant's size and surface properties. The presence of FBGCs and monocytes/macrophages may influence the strength of the implant-tissue integration and more monocytes/macrophages have been found to rest on smooth surfaces than on rough surfaces (Anderson, 2000). It has been further shown that surface smoothness may induce the differentiation of cells of the monocytic lineage and the formation of FBGCs out of the ce...