- English
- ePUB (mobile friendly)
- Available on iOS & Android
Clinical Cardiac Electrophysiology Handbook, Second Edition
About This Book
The Clinical Cardiac Electrophysiology Handbook, Second Edition, is a concise presentation in outline format of the practical information needed to understand the subtleties of cardiac electrophysiology. The Handbook focuses on the "how-to" management of arrhythmias, along with an understanding of the "why.""... a quick source for information in the EP lab or on the wards offering the ability to quickly review the essential components before a case or to reinforce new notions and practices encountered during a case." — From the Preface Fully illustrated with more than 250 figures and tables. Equally valuable to the cardiology fellow on their electrophysiology rotation, or an EP fellow or technologist working in the EP lab.New and updated sections in the Second Edition: Ablation energy and biophysics, including pulsed field ablation AF ablation techniques adjunctive to pulmonary vein isolation Alternatives to cardiac resynchronization therapy His bundle pacing Intracardiac echocardiography Left atrial appendage occlusion
Frequently asked questions
Information
CHAPTER
1
Fundamentals
THE CARDIAC ACTION POTENTIAL
- Automaticity: The ability to initiate an impulse or stimulus. In the absence of external stimulation, the pacemaker cells spontaneously depolarize. This property generates sinus rhythm at a rate appropriate to the body’s needs.
- Excitability: The ability to respond to an impulse or stimulus. Myocardial cells respond to the impulse generated by the pacemaker cells of the cardiac conduction system through depolarization and repolarization.
- Conductivity: The ability to transmit impulses to other areas. While conductivity is much more efficient in the conduction system, the cells in the conduction system and the myocardium also have this property.
- Refractoriness: The property that governs the time following excitation until the tissue can be re-excited. This property prevents tissue from being re-excited too soon after the previous excitation, thereby protecting against dangerously rapid rates and reentrant arrhythmias.
- Contractility: The ability to respond to electrical stimulation with mechanical action.
The “Fast-Channel” Cardiac Action Potential
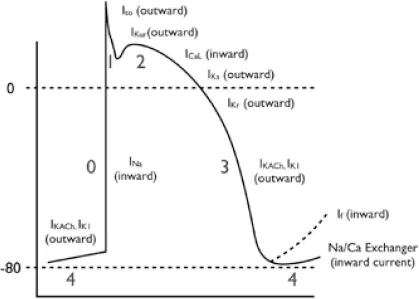
Depolarization
- Phase 0: Rapid depolarization phase (“upstroke”)
- With stimulation, the fast sodium (Na) channels are activated, resulting in a rapid increase in sodium membrane conductance (GNa) and/or rapid influx of sodium ions (INa) into the cell.
- The entry of positively charged sodium ions produces a rapid change in the electrical charge of the interior of the cell, providing the energy for rapid impulse propagation.
Repolarization
- Phase 1: Early repolarization The early repolarization phase starts with the opening of rapid, outward potassium current (Ito). This currents result in rapid repolarization to about 0 mV.
- Phase 2: “Plateau” phase A “stable” membrane potential is observed resulting from a balance of the inward movement of calcium through L-type calcium channels (ICa,L) and the outward movement of K+ through the delayed rectifier (rapid and slow components: IKr and IKs) and the inward rectifier (IK1) potassium channels. The sodium–calcium exchange current (INa/Ca) and the sodium–potassium pump current (INa/K) also play minor roles in the maintenance of the current, and major roles in the maintenance of physiological intracellular sodium, potassium, and calcium concentrations.
- Phase 3: Rapid repolarization at the conclusion of the plateau phase Initially, the net negative change in membrane potential is driven by the inactivation of L-type Ca channels. The rapid delayed rectifier K+ channel (IKr) and inwardly rectifying K+ current (IK1) activate, causing a more rapid net outward current, causing the cell to repolarize to baseline. This phase governs refractoriness by controlling action potential duration (APD). INa is inactivated at voltages positive to –60 mV, so following the phase 0 upstroke, the cell cannot be reactivated until it returns to –60 mV during phase 3. The APD to –60 mV determines the “effective refractory period” (ERP) of fast-channel tissue.
- Phase 4: Resting phase The resting phase constitutes a steady, stable, polarized membrane (–90 mV in working myocardial cells). When membrane potential is restored to baseline, the delayed rectifier K+ channels close. Voltage-regulated inward rectifiers (IK1) remain open, regulating resting membrane potential.
Ventricular Action Potential
- Longer duration
- Higher phase 2 (absent IKur)
- Shorter phase 3, with faster repolarization
Action Potential of the His-Purkinje System
- More prominent early (phase 1) repolarization
- Longer plateau phase (phase 2)
- Automaticity: Spontaneous, phase 4 depolarization
The “Slow-Channel” Cardiac Action Potential
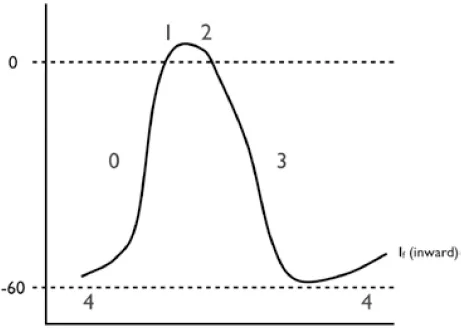
- Phase 0: Rapid depolarization phase (“upstroke”) This phase is slower (conduction velocity of ~0.02 to 0.05 m/s) due to a smaller inward current that governs activation (generated by ICa,L, rather than INa).
- Phase 1: Early repolarization phase Early repolarization is not perceptible in slow-channel tissue, because Ito is small and partially inactivated by the relatively positive resting potential.
- Phase 2: “Plateau” phase In principle, this phase is similar to that of fast-channel tissue, except that because of the small phase 0 current, the transitions from phase 0 to phase 1 and subsequently to phase 2 are much less defined.
- Phase 3: Rapid repolarization at the conclusion of the plateau phase This phase has similar ionic mechanisms to fast-channel phase 3. Because ICa,L is smaller and recovers much more slowly than INa, the main factor determining ERP in slow-channel tissue is slow, time-dependent recovery of ICa,L. Therefore, unlike fast-channel tissue, APD is not the main determinant of ERP and changes in APD have relatively little effect on ERP. The time-dependent recovery of ICa,L results in reduced current at fast rates, greatly limiting the maximum follow frequency of the AVN. This is an important protective property that prevents excessively rapid ventricular rates during very rapid supraventricular tachyarrhythmias like atrial flutter (AFL) and atrial fibrillation (AF).
- Phase 4: “Resting” phase Automaticity results from the combination of: (1) spontaneous diastolic depolarization due to phase 4 If (a poorly selective, inward current carried mainly by Na and activating upon repolarization), activation of T-type Ca2+ current (ICa,T), and inactivation of delayed rectifier K+ currents; and (2) the maximum negative “resting” potential (“maximum diastolic potential” or MDP) being closer to the depolarization threshold (–50 to –60 mV vs. –80 mV for fast-channel potentials).
ARRHYTHMIA MECHANISMS
General Classification of Arrhythmia Mechanisms
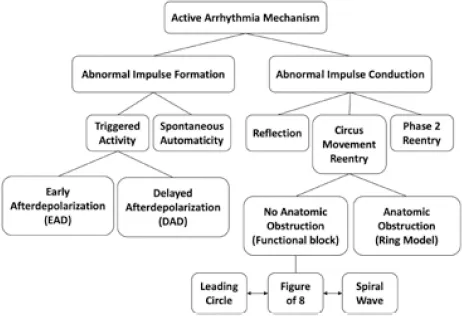
Altered Impulse Formation
Automaticity
- Driven by spontaneous, phase 4 depolarization.
- May be influenced by neurohormonal (s...
Table of contents
- Cover Page
- Title Page
- Copyright
- Contents
- About the Authors
- Preface to the First Edition
- Preface to the Second Edition
- Abbreviations
- 1 Fundamentals
- 2 Electrophysiology Study and Maneuvers
- 3 Electrophysiology Study: Specific Approaches
- 4 Atrioventricular Nodal Reentrant Tachycardia
- 5 Accessory Pathways
- 6 Atrioventricular Reciprocating Tachycardia
- 7 Focal Atrial Tachyarrhythmia
- 8 Atrial Flutter and Macroreentrant Atrial Tachycardia
- 9 Atrial Fibrillation
- 10 Ventricular Tachycardia
- 11 Sinus Tachycardia
- 12 Bradycardia and Blocks
- 13 Cardiac Implantable Electronic Devices
- 14 Sudden Cardiac Death and Inherited Arrhythmias
- 15 Syncope
- Index