![]()
Chapter 1
Overview of Physician Affiliation Options—50 Years of History
Through the years, the presence of physicians, hospitals, and other healthcare investors or partners has increased the complexity of the healthcare delivery system to what it is today. Though not entirely extinct, single-ownership physician practices, small locally owned hospitals, and other private healthcare entities are rare in today’s multifaceted organizations. Providers at all levels are compelled to affiliate with others to function and thrive in such a complex environment, and the options for affiliation seem almost endless.
In this chapter, we will consider how we arrived at the current array of affiliation models. They did not emerge overnight; they are the result of literally decades of societal and economic issues and realities that have changed the healthcare landscape in America, including the increased involvement of state, local, and federal governments.
We learn from history; thus, we begin by looking back 50 years and working our way to the present. Some of the models we discuss in the following chapters have been around for years; they are merely repackaged to be more responsive to present-day settings. Others are newer and a reflection of the dynamics within our healthcare industry, which is still largely private-entity-based.
Additionally, our healthcare providers (mostly hospitals and health systems) are significantly represented as not-for-profit, tax-exempt entities. Physicians and related providers, if private, are likely for-profit entities, but they work closely across the aisle with not-for-profits. When they become fully affiliated/aligned with not-for-profit health systems, however, they may not be officially not-for-profit entities. Likewise, for-profit health systems should be considered within the various transactional structures of affiliation.
Finally, there is an abundance of private practicing physician groups and related ancillary service entities. Note: In this context, we define ancillary service entities as those that provide healthcare services directly to the provision of professional care, but ancillary services are in addition to (and billed as such) professional services. Examples include imaging, surgical, and diagnostic testing services.
With history as a basis, let’s explore how the past has shaped our current (and projected future) landscape regarding affiliation models and associated transactions. By definition, we are broadening our consideration of transactional relationships to include physicians and hospitals/health systems; physicians with other physicians; physicians and health systems with for-profit investor entities, including private equity (PE) firms; and all other forms of potential affiliation, including insurance companies/payers. In short, the universe of potential partners in today’s healthcare affiliation transactions has virtually no limitations.
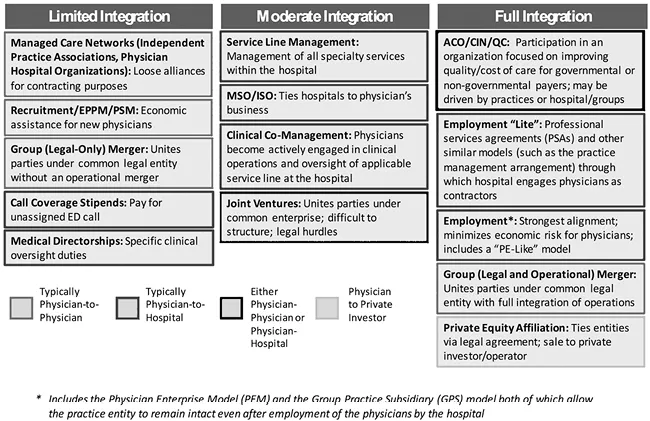
Figure 1.1. Traditional Alignment Model Descriptions
Figure 1.1 serves as the foundation for this discussion and is referenced in detail as we explore the specific models presented throughout this book. Moreover, all these examples are applicable as we consider the history of transactional affiliation models. Many are not new or untried, though some are more recently developed and incorporated in the transactional affiliation structures.
Now, let’s take a walk down memory lane and consider how our healthcare system has changed in the context of physicians and related providers and their affiliation structures over the past 50 years.
The 1970s and 1980s
We group these two decades because they have similar characteristics relative to affiliation transaction models and structures. The U.S. economy during the 1970s was somewhat volatile, with high interest rates and inflationary economic trends. The economy slowed in the latter part of the 1970s, with inflation and interest rates often reaching double digits. Economic trends improved in the 1980s, allowing greater affluence and better financial times. Overall, the healthcare industry mirrored these trends.
With this economic backdrop, the relationships between healthcare providers—physicians and hospitals/health systems—were mostly at arm’s length. Transactional integration was rare. Most physicians were in private practice; many were in small groups or solo practices. Physicians who were just out of training and ready to start their career in medicine generally considered two options: working within a private group with aspirations to become a partner within that group or starting a solo practice.
Although some physicians practiced in larger groups, little emphasis was placed on mergers. The reimbursement model was fee-for-service, though some areas of the country introduced risk-based contracts tied mostly to capitated models, also called managed care, in the late 1980s. Typically, the capitation models were with primary care; specialists were rarely involved in capitation arrangements. (See “A Short History of Managed Care” in the sidebar.)
Hospitals were keenly aware of the need to work with physicians and allied healthcare providers, but the relationship was mostly through medical staff membership and more distant affiliations. Referring to Figure 1.1, the relationships among physicians and hospitals are captured in the Limited Integration column. Many physicians were members of medical staffs of various hospitals—usually competing facilities. Physicians may have looked to hospitals for financial assistance but usually in the context of recruitment support and/or medical directorships and possibly some compensation for specific contracted services, depending on the specialty and overall needs of the hospital. There were few mega-groups. Some multi-specialty groups existed and even a few larger single-specialty groups; however, private practicing physicians’ ability to realize a level of reimbursement that allowed them an acceptable bottom line (i.e., take-home pay) left few desiring anything more than an at-arm’s-length relationship with hospitals. Similarly, hospitals saw no pressing need to employ or closely integrate with physicians.
Hospitals were more concerned about medical staff relations and overall responsiveness to their physicians who often had a choice of which competitive hospital facility to work with and refer their patients to. Consequently, hospitals became acutely aware of the need to provide customer service to private physician groups through improved responsiveness and support of the patients the physicians admitted to the hospital, which was not the typical model at the time (see “Hospital of Yesterday: The Biggest Changes in Healthcare” sidebar). Fewer outpatient services were provided than is currently the case. The delivery of inpatient services that called for inpatient stays was still the dominant form of care, especially in surgical cases (see “Long Stays” sidebar.)