- English
- ePUB (mobile friendly)
- Available on iOS & Android
Pain Medicine at a Glance
About This Book
Pain Medicine at a Glance
The market-leading at a Glance series is popular among healthcare students and newly qualified practitioners for its concise, simple approach and excellent illustrations.
Each bite-sized chapter is covered in a double-page spread with clear, easy-to-follow diagrams, supported by succinct explanatory text.
Covering a wide range of topics, books in the at a Glance series are ideal as introductory texts for teaching, learning and revision, and are useful throughout university and beyond. Everything you need to know about Pain Medicine... at a Glance!
Pain Medicine at a Glance is a user-friendly, visual introduction to the impact of pain in various clinical care settings, focusing on primary care needs. Aligned with learning objectives developed by the Johns Hopkins School of Medicine, this authoritative guide covers the basic forms and pathophysiology of pain, the clinical skills necessary for delivering excellent care, pharmacological and non-pharmacological treatments, and a variety of special cases such as healthcare ethics, integrative care, and treatment planning for chronic pain self-management therapy and the management of pain in children and older adults.
A new addition to the market-leading at a Glance series, the text offers concise and accessible chapters, full-color illustrations, self-assessment questions, and easy-to-follow diagrams. Topics include pain assessment, cognitive factors that influence pain, applying behavioral perspectives on pain, managing opioids and other pharmacological therapies, treating acute pain in patients with substance abuse issues, and more. Perfect for learning, revision, and teaching, this book:
- Provides a foundation of clinical and basic science knowledge about pain and its mechanisms
- Describes major forms of pain, including surgical, orofacial, musculoskeletal, and obstetric pain
- Offers advice on fostering empathy and compassionate practices in pain medicine
- Covers non-pharmacological treatments such as physical therapy, hydrotherapy, meditation, acupuncture, massage, and various focal treatments
- Includes discussion of recent advances and new discoveries in pain science
Pain Medicine at a Glance is the ideal companion for medical and healthcare students, junior doctors, advanced practice providers, nurse practitioners, and others involved in diagnosing and treating pain-associated illness.
For more information on the complete range of Wiley medical student and junior doctor publishing, please visit: www.wiley.com
To receive automatic updates on Wiley books and journals, join our email list. Sign up today at www.wiley.com/email
All content reviewed by students for students
Wiley Medical Education books are designed exactly for their intended audience. All of our books are developed in collaboration with students. This means that our books are always published with you, the student, in mind.
If you would like to be one of our student reviewers, go to www.reviewmedicalbooks.com to find out more. This book is also available as an e-book. For more details, please see www.wiley.com/buy/9781118837665
Frequently asked questions
Information
1
What is pain and how do we assess it?
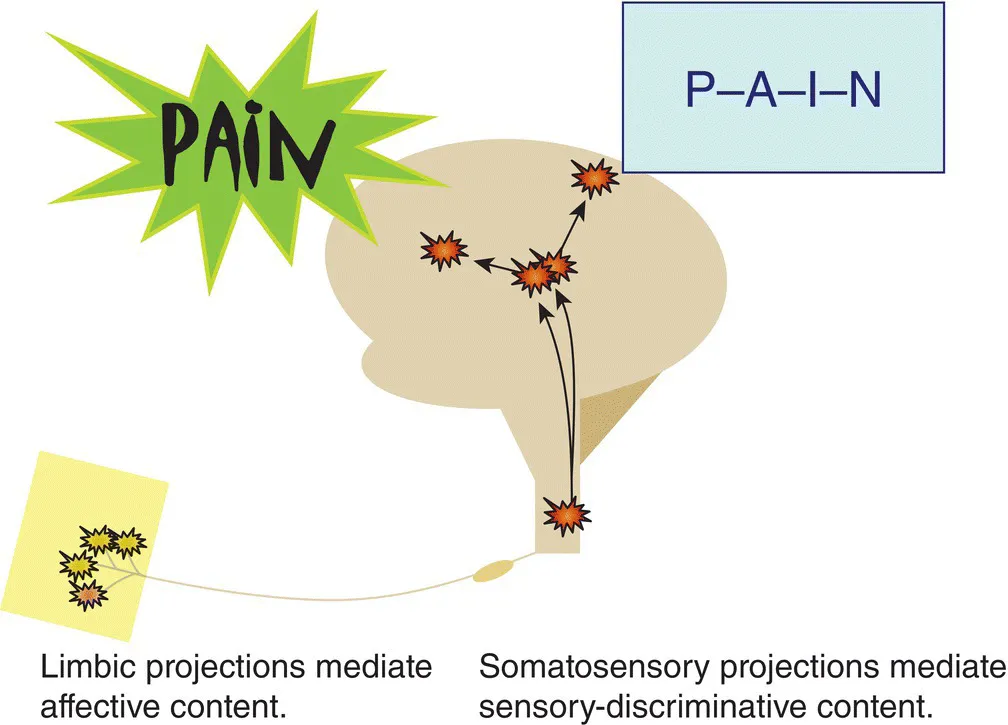
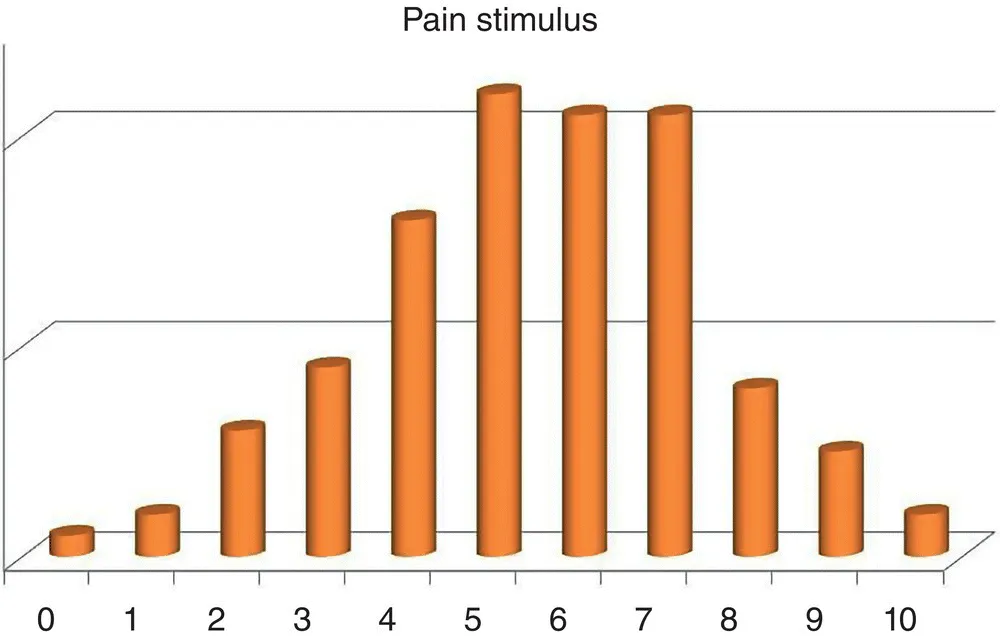
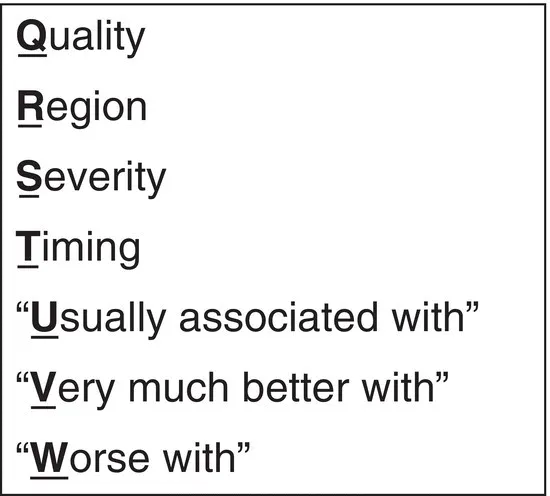
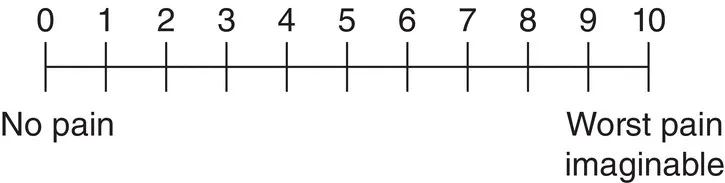
Table of contents
- Cover
- Table of Contents
- Title Page
- Copyright Page
- Dedication Page
- Preface
- Foreword
- Acknowledgment
- 1 What is pain and how do we assess it?
- 2 Nociceptive processing
- 3 What are the major types of pain?
- 4 How prevalent is pain and what are the common forms?
- 5 Pain and ethical practice
- 6 Advanced skillfulness in clinical practice
- 7 Cognitive factors that influence pain
- 8 Approach to the patient with pain
- 9 The pain‐focused clinical history
- 10 Assessing pain in those with communication barriers
- 11 Examination skills I
- 12 Examination skills II
- 13 Integrating knowledge, skills, and compassionate practices
- 14 Motivational interviewing and shared decision‐making
- 15 Communication and interprofessional teams caring for patients with pain
- 16 Planning therapy
- 17 Basic considerations for pharmacological therapy – balancing mechanisms of drugs and disease
- 18 Over‐the‐counter analgesia
- 19 Neuromodulating agents
- 20 Opioids – the basics and use in perioperative pain care
- 21 Opioids – the details
- 22 Opioids – advanced practice – alternative delivery routes
- 23 Focal treatments for pain in primary practice
- 24 Interventional treatments and surgery for pain
- 25 Activating therapies
- 26 Mind‐based therapies
- 27 Manual therapies: massage; trigger points, acupressure, chiropractic, stretching, inversion
- 28 Therapies that utilize descending pain pathways: meditation, vocation, games, music, and others
- 29 Acute and chronic pain: the basics
- 30 Surgical and procedural pain
- 31 Musculoskeletal pain
- 32 Orofacial pain
- 33 Neck pain, cervical, and thoracic spine pain
- 34 Arm and hand pain
- 35 Low back pain
- 36 Back pain emergencies
- 37 Radiating leg, buttock, and groin pain
- 38 Knee pain
- 39 Foot and ankle pain
- 40 Headache emergencies
- 41 Headaches
- 42 Headache – chronic pain and the acute flare
- 43 Visceral pain
- 44 Pelvic pain
- 45 Exceptional causes of severe, chronic pain
- 46 Management of pain in those with substance abuse
- 47 Pain at the end of life, opioid rotation
- 48 Opioids for chronic pain: preventing iatrogenic opioid use disorders
- 49 Tapering opioids in patients with pain
- 50 Pain in infants, children, and adolescents
- 51 Pain in older adults
- 52 Tailoring pharmacotherapy in aging, renal, liver, and other metabolic dysfunctions
- 53 Pain in pregnancy and the puerperium
- References
- Appendix I: Sample exam sheet
- Appendix II: Sample pain diary worksheet
- Appendix III: Glossary
- Appendix IV: Daily stretching guide – essential for pain prevention
- Appendix V: Patient packet – your power over pain
- Multiple choice questions
- Answers
- Index
- End User License Agreement