- 218 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
About This Book
Maybe we have an obsession for cases, but when we were resident in radiology, we loved to learn especially from cases not only because they are short, exciting and fun, similar to a detective story in which the aim is to get to 'the bottom' of the case, but also because, in the end, that's what radiologists are faced with during their daily work.
The topics covered in the book represent the common and important diseases encountered in abdominal and pelvic imaging. The material presented for each case provides a thorough and comprehensive description of the disease entity, enabling the radiologist or the clinician to develop a clear concept of the entity through the different imaging modalities that are present. What is interesting in this book is one case per page. The book can be used as a means of rapid revision of a large number of cases in a short time or as test of knowledge by masking the radiological description and diagnosis and trying by using the clinical data and radiological images to describe first the pathology then propose a diagnosis.
Frequently asked questions
Information
Case 1
-
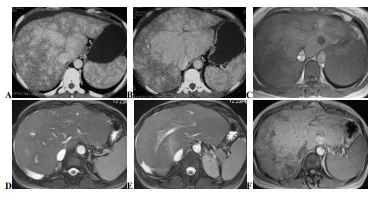
Enhanced CT scan, axial (A, B) and MR scan, axial T1 (C), axial T2 fat saturation (D, E) and post-contrast axial T1 (F) images. On CT images, the liver is enlarged with hypertrophied caudate lobe: mottled enhancement with prominent enhancement of the central liver and decreased enhancement of the liver periphery (nutmeg liver). The areas of decreased enhancement are due to decreased portal flow, hepatic congestion and ischemia. Non-visualisation of the hepatic veins. The MR sequences show the same appearances with homogeneous liver on T2 and enhancement of the central liver (the caudate lobe enhances normally as it has a separate draining vein directly into the inferior vena cava) with decreased signal intensity of the atrophied liver periphery. The IVC is patent. Note mild ascites.
Case 2
-
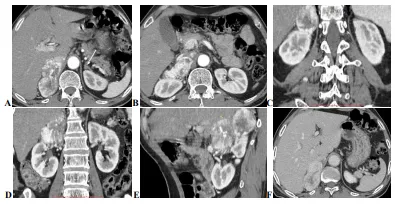
Enhanced abdominal CT scan, post-contrast arterial phase axial (A, B) / coronal and sagittal reconstruction (C, D, E) and post-contrast portal phase axial (F) images reveal a well-defined lobulated right suprarenal mass with intense and heterogeneous enhancement and prominent surrounding vessels on arterial phase and rapid washout on portal phase. Note the IVC is displaced anteriorly and the upper pole of the kidney posteriorly. The left adrenal gland appears normal in size and shape (arrow image A).
Case 3
-
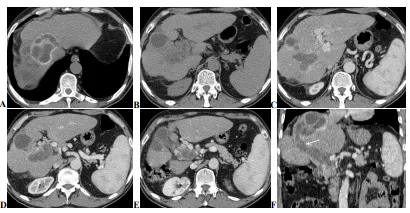
Pre-(A, B) and post-contrast (C, D, E) abdominal CT scan with coronal reconstruction (F) images showing a dysmorphic liver (past history of surgery for hydatid cysts) with hydatid cysts located in the segments, VIII/VII (CE4 and CE3A, WHO classification) and V (CE3 A, WHO classification). The portal vein and its right branch are dilated, containing germinative membranes and other cyst contents with evidence of fistulous tract between the hydatid cyst located in the segment VIII and dilated right branch of portal vein (arrow in F). Note the presence of tortuous venous structures around the thrombosed portal vein indicating portal cavernoma. The spleen was moderately enlarged with dilated splenic vein (extra-hepatic portal hypertension).
Case 4
-
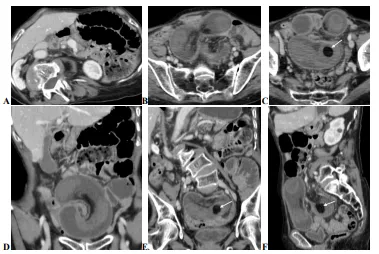
Enhanced Abdominal CT scan, axial (A, B, C) with coronal / sagittal reconstruction (D, E, F) images showing a sausage-shaped mid-pelvic mass with central area containing mesenteric fat and vessels indicating intussusception. Distal within this mass there is a well-defined fatty-density lesion (arrow images, C, E and F) representing a lipoma. Note proximal small bowel dilatation.
Case 5
-
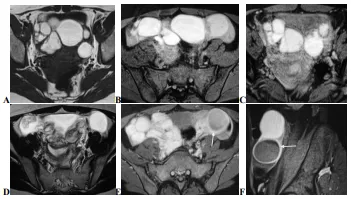
MR scan, axial T1 (A), T1 fat saturation (B, C), axial T2 (D) and post-contrast axial / sagittal T1 fat saturation (E, F) images showing multiple and bilateral well-circumscribed contiguous ovarian cystic lesions of high signal intensity on T1 and T1 fat saturation, low signal intensity on T2 with no peripheral enhancement after gadolinium administration (endometriomas). Both ovaries are closed up due to interovarian adhesions (Kissing ovaries). Note that the left ovary shows also another cystic lesion of high signal intensity on T1 and T2 with peripheral regular enhancement after gadolinium administration (haemorrhagic cyst, arrow in E and F). The uterus was normal.
Case 6
-
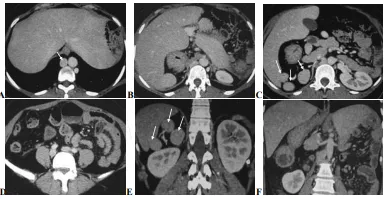
Enhanced abdominal CT scan, axial (A, B, C, D) with coronal reformatted (E, F) images. The liver is in midline (or bridging liver) with stomach on the right side. Three splenules are seen on the right below the liver (arrows in C and E) with no splenic structure seen in the left hypochondrium. Note an interruption of the inferior vena cava with azygous continuation of the IVC (arrow in A). The head and the corporeo-caudal region of the pancreas are on the right, giving the appearance of a lying V (image C) with Preduodenal position of the portal vein. The duodenojejunal junction does not cross the midline; it should be located on the same side of the body as the stomach and approximately at the level of the duodenal bulb, indicating associated intestinal malrotation.
Case 7
Table of contents
- Abdominal-Pelvic Imaging
- About the Author
- Dedication
- Copyright Information ©
- Acknowledgements
- Foreword
- Preface
- Case 1
- Case 2
- Case 3
- Case 4
- Case 5
- Case 6
- Case 7
- Case 8
- Case 9
- Case 10
- Case 11
- Case 12
- Case 13
- Case 14
- Case 15
- Case 16
- Case 17
- Case 18
- Case 19
- Case 20
- Case 21
- Case 22
- Case 23
- Case 24
- Case 25
- Case 26
- Case 27
- Case 28
- Case 29
- Case 30
- Case 31
- Case 32
- Case 33
- Case 34
- Case 35
- Case 36
- Case 37
- Case 38
- Case 39
- Case 40
- Case 41
- Case 42
- Case 43
- Case 44
- Case 45
- Case 46
- Case 47
- Case 48
- Case 49
- Case 50
- Case 51
- Case 52
- Case 53
- Case 54
- Case 55
- Case 56
- Case 57
- Case 58
- Case 59
- Case 60
- Case 61
- Case 62
- Case 63
- Case 64
- Case 65
- Case 66
- Case 67
- Case 68
- Case 69
- Case 70
- Case 71
- Case 72
- Case 73
- Case 74
- Case 75
- Case 76
- Case 77
- Case 78
- Case 79
- Case 80
- Case 81
- Case 82
- Case 83
- Case 84
- Case 85
- Case 86
- Case 87
- Case 88
- Case 89
- Case 90
- Case 91
- Case 92
- Case 93
- Case 94
- Case 95
- Case 96
- Case 97
- Case 98
- Case 99
- Case 100
- Case 101
- Case 102
- Case 103
- Case 104
- Case 105
- Case 106
- Case 107
- Case 108
- Case 109
- Case 110
- Case 111
- Case 112
- Case 113
- Case 114
- Case 115
- Case 116
- Case 117
- Case 118
- Case 119
- Case 120
- Case 121
- Case 122
- Case 123
- Case 124
- Case 125
- Case 126
- Case 127
- Case 128
- Case 129
- Case 130
- Case 131
- Case 132
- Case 133
- Case 134
- Case 135
- Case 136
- Case 137
- Case 138
- Case 139
- Case 140
- Case 141
- Case 142
- Case 143
- Case 144
- Case 145
- Case 146
- Case 147
- Case 148
- Case 149
- Case 150
- Case 151
- Case 152
- Case 153
- Case 154
- Case 155
- Case 156
- Case 157
- Case 158
- Case 159
- Case 160
- Case 161
- Case 162
- Case 163
- Case 164
- Case 165
- Case 166
- Case 167
- Case 168
- Case 169
- Case 170
- Case 171
- Case 172
- Case 173
- Case 174
- Case 175
- Case 176
- Case 177
- Case 178
- Case 179
- Case 180
- Case 181
- Case 182
- Case 183
- Case 184
- Case 185
- Case 186
- Case 187
- Case 188
- Case 189
- Case 190
- Case 191
- Case 192
- Case 193
- Case 194
- Case 195
- Case 196
- Case 197
- Case 198
- Case 199
- Case 200