![]()
Levy-Marchal C, Pénicaud L (eds): Adipose Tissue Development: From Animal Models to Clinical Conditions.
Endocr Dev. Basel, Karger, 2010, vol 19, pp 1–20
______________________
Human Lipodystrophies: Genetic and Acquired Diseases of Adipose Tissue
Jacqueline Capeaua-c · Jocelyne Magréa,b · Martine Caron-Debarlea,b · Claire Lagathua,b · Bénédicte Antoinea,b · Véronique Béréziata,b · Olivier Lascolsa-c · Jean-Philippe Bastarda-c · Corinne Vigourouxa-c
aINSERM, U938, CDR Saint-Antoine; bUPMC University Paris 06, UMR_S938 and cAP-HP Tenon and Saint-Antoine Hospitals, Paris, France
______________________
Abstract
Human lipodystrophies represent a heterogeneous group of diseases characterized by generalized or partial fat loss, with fat hypertrophy in other depots when partial. Insulin resistance, dyslipidemia and diabetes are generally associated, leading to early complications. Genetic forms are uncommon: recessive generalized congenital lipodystrophies result in most cases from mutations in the genes encoding seipin or the 1-acyl-glycerol-3-phosphate-acyltransferase 2 (AGPAT2). Dominant partial familial lipodystrophies result from mutations in genes encoding the nuclear protein lamin A/C or the adipose transcription factor PPARγ. Importantly, lamin A/C mutations are also responsible for metabolic laminopathies, resembling the metabolic syndrome and progeria, a syndrome of premature aging. A number of lipodystrophic patients remain undiagnosed at the genetic level. Acquired lipodystrophy can be generalized, resembling congenital forms, or partial, as the Barraquer-Simons syndrome, with loss of fat in the upper part of the body contrasting with accumulation in the lower part. Although their etiology is generally unknown, they could be associated with signs of autoimmunity. The most common forms of lipodystrophies are iatrogenic. In human immunodeficiency virus-infected patients, some first-generation antiretroviral drugs were strongly related with peripheral lipoatrophy and metabolic alterations. Partial lipodystrophy also characterize patients with endogenous or exogenous long-term corticoid excess. Treatment of fat redistribution can sometimes benefit from plastic surgery. Lipid and glucose alterations are difficult to control leading to early occurrence of diabetic, car-diovascular and hepatic complications.
Copyright © 2010 S. Karger AG, Basel
Diseases of adipose tissue are present with a high prevalence in the global population, in particular those linked with fat expansion leading to obesity, metabolic syndrome or type 2 diabetes. The consequences of increased fat depots are markedly dependent upon their localization. Adipose tissue in the lower part of the body is able to expand and can therefore accumulate excessive energy from diet, stored as triglycerides: taken as a whole, it appears protective at the metabolic level [1]. By contrast, accumulation of fat in the upper part of the body is deleterious. Most abdominal fat is accounted for by subcutaneous fat (SAT) and, under physiologic conditions, only a minor part is represented by intra-abdominal visceral fat (VAT). Excessive SAT, and even more VAT, is strongly associated with metabolic alterations and insulin resistance. These alterations result from the increased release of free fatty acids (FFA) from insulin-resistant adipocytes but also from modified adipokine production with decreased production of adiponectin by adipocytes and increased production of pro-inflammatory cytokines (IL-6, IL-1β, TNF-β) and chemokines (such as CCL2), in part by adipocytes, but mainly by macrophages invading adipose tissue [2].
Human lipodystrophies are far less common than obesity and characterized, at the opposite, by fat disappearance. However, at the metabolic level, common alterations are observed with insulin resistance, dyslipidemia and generally increased FFA and decreased adiponectin production. Recently, the genetic origin of some of these lipodystrophies has been clarified. However, a number of patients remain undiagnosed at the genetic level. Otherwise, some acquired forms are iatrogenic [3–6].
Definition and Diagnosis
Human lipodystrophies represent a heterogeneous group of diseases [4–6] characterized by the loss of body fat, which could be localized or generalized. If localized, it is often associated with fat hypertrophy in some other depots.
At the clinical level, peripheral lipoatrophy affecting SAT can be easily diagnosed when marked and affecting regions with a natural large fat thickness. Loss of fat into cheeks and temples gives a gaunt face and, in the limbs, makes muscles and veins highly visible. However, lipoatrophy can be difficult to diagnose if mild, in particular at the lower limb level in males, who can have physiologically a low fat amount. In those cases, a CT scan at the thigh level is useful but requires comparisons with normal subjects. The diagnosis of visceral fat atrophy (or hypertrophy) requires imaging techniques: a CT scan or a MRI at the lumbar L4 level allows precise evaluation of the SAT and VAT areas.
Human lipodystrophies are generally associated with severe insulin resistance. Therefore, clinical signs of insulin resistance can help diagnosis: the presence of skin lesions of acanthosis nigricans, a skin-brownish lesion present in the axillae, neck and other body folds is an excellent indication of marked insulin resistance, in particular in normal-weight patients. Long-term insulin resistance can lead to acromegaloid features, striking in face and seen in particular in congenital forms. Insulin resistance can result in increased size of genital organs in prepubertal children, ovarian hyperandrogenism leading to virilization and hirsutism with polycystic ovary syndrome and hyperthecosis in women. Insulin resistance is also commonly associated with hepatomegaly and steatosis.
At the metabolic level, lipodystrophies are characterized by glucose and lipid alterations which can be mild or even absent during childhood and increase in severity when patients age. Lipid alterations associate increased triglyceride (TG) level, which can be raised up to 100 mmol/l, leading to a high risk of acute pancreatitis, while HDL cholesterol is decreased. Glucose values could remain in the normal range in young patients, if insulin secretion is able to compensate for insulin resistance, but increase progressively leading to glucose intolerance then diabetes, difficult to control.
The main acute complication is acute pancreatitis due to very high TG level. Chronic complications are related to long-term diabetic complications, microangiopathy, affecting retina, kidney and nerves, macroangiopathy, leading to early atherosclerosis, and to hepatic complications of steatosis leading to steatohepatitis and sometimes cirrhosis and portal hypertension.
The differential diagnosis with syndromes of insulin resistance due to alterations at the insulin receptor level (leprechaunism, type A and type B syndromes) could be difficult. However, in these later syndromes, lipodystrophy and dyslipidemia are absent and very high adiponectin levels have been recently reported [7]. Lipomatosis represents localized fat tumors, different from lipodystrophies. They can be multiple, affecting mainly the proximal limbs areas and the neck in the familial lipomatosis, and are sometimes associated with mutations in mitochondrial DNA (MERRF mutations in particular). The Launois-Bensaude lipomatosis, of unknown origin, is often associated with peripheral neuropathy and increased alcohol intake.
Classification
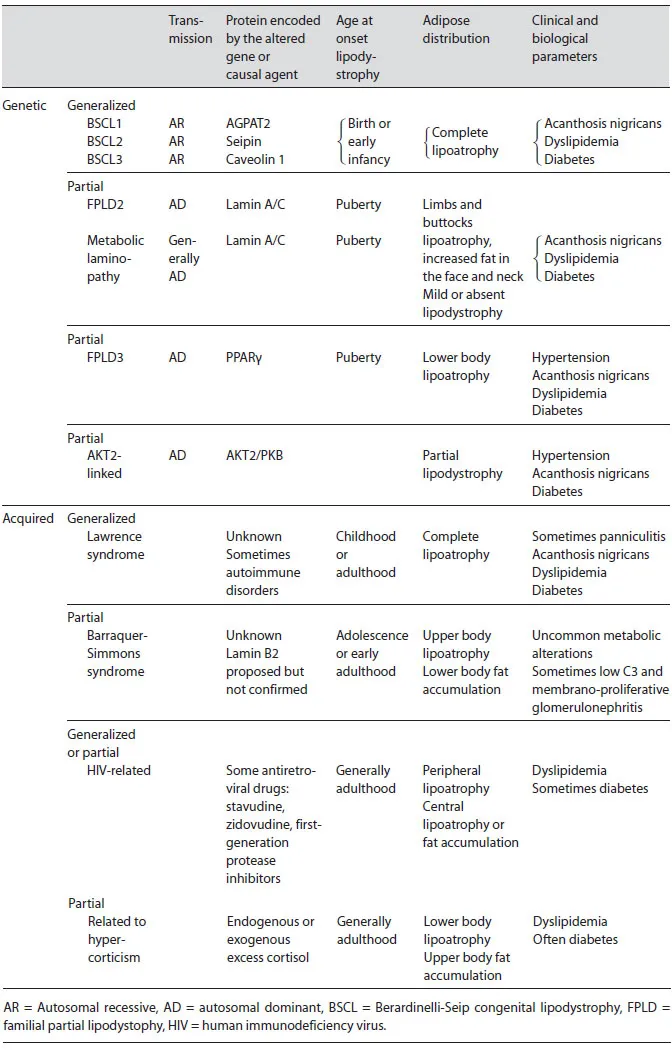
Human lipodystrophies can be defined by the extent of fat loss (generalized or partial) and by their etiology, either genetic or acquired (table 1). Genetic forms of lipodystrophy are uncommon diseases and, up to now, only a few genes have been identified, the alteration of which is responsible for lipodystrophy and insulin resistance.
Genetic forms of complete lipodystrophy called Berardinelli-Seip congenital lipodystrophy (BSCL) or congenital generalized lipodystrophy are exceptional, with fat loss being generally recognized at birth or very early in infancy. It is associated with severe insulin resistance. Most of the patients present recessive mutations in one of two genes, BSCL2 encoding seipin or 1-acyl-glycerol-3-phosphateacyltransferase-2 (AGPAT2). A third gene, CAV1, encoding caveolin 1, has been recently identified in one patient. At present, less than 5% of patients with congenital generalized lipodystrophy remain without identified genetic alteration.
Table 1. Classification and main clinical features of lipodystrophies
In partial lipodystrophies, which are rare diseases, two major genes have been identified so far that present generally heterozygous mutations: LMNA, encoding lamin A/C and PPARG encoding PPARγ. Mutations in LMNA are more frequent than those in PPARG and can lead to a number of phenotypes, among which a phenotype where severe insulin resistance is the dominant feature, now designed as ‘metabolic laminopathy’ [8]. In an international effort searching for new disease-causative genes, mutations in AKT2, LMNB2 encoding lamin B2, CAV1 and CIDEC were reported in a few patients which remain isolated cases. Numerous patients remain undiagnosed at the genetic level.
Those observed in human immunodeficiency virus (HIV)-infected patients and attributed to the antiretroviral treatment mainly represent acquired forms of lipodystrophy. Very recent data suggest that the chronic viral infection could be also involved. New antiretroviral drugs, with less adverse effects on adipose tissue, are now used. Therefore, lipodystrophy is now less prevalent in this population. However, a number of comorbidites related to insulin resistance and aging occur at an early age in these patients.
A number of acquired lipodystrophies have been recognized for a long time in some rare patients. These forms can be either generalized, as the Lawrence syndrome, or partial, as the Barraquer-Simons syndrome. Their origin is unknown even if immune alterations and signs of autoimmunity have been indentified in some patients. Otherwise, patients with hypercortisolism, either endogenous or exogenous, often present fat redistribution with loss of fat in the limbs and buttocks and increased fat in the upper part of the body, and in particular at the back of the neck (buffalo hump).
Finally, fat redistribution with loss of fat in the periphery and increased fat at the central level, is a physiologic evolution during aging. This central fat redistribution is associated with metabolic alterations such as insulin resistance, increased prevalence of diabetes and dyslipidemia. This could represent a very mild and physiologic form of lipodystrophy with associated metabolic abnormalities. This central fat redistribution is exacerbated in the metabolic syndrome with associated metabolic alterations leading to an increased risk of cardiovascular disease and of diabetes.
Pathophysiology of Adipose Tissue Loss
Adipose tissue now appears as playing a leading role in energy metabolism and insulin sensitivity through the control of lipid metabolism and the secretion of numerous adipokines involved in important functions and in particular in insulin sensitivity (mainly adiponectin) and insulin resistance (pro-inflammatory cytokines). When fat depots are reduced due to lipoatrophy, as seen in these patients, TG present on circulating lipoproteins, chylomicrons and VLDL can be only partially stored in fat depots leading to increased circulating TG [9]. In addition, the hydrolysis of TG on lipoproteins, occurring inside the vascular lumen, leads to increased circulating FFA levels. Reduced fat amounts result in reduced circulating leptin [10] levels that are strongly related to the total amount of fat and in particular of SAT. Very low levels of leptin are deleterious for metabolism and leptin replacement therapies were shown to markedly improve metabolic parameters in patients with severe lipodystrophies. Adiponectin values are also generally greatly reduced [10] in association with strong insulin resistance. Adiponectin is important to oxidize FFA into mitochondria in the liver and muscles. Therefore, adiponectin deficiency impairs this oxidation leading to intracellular accumulation of fatty acid derivatives. Increased FFA and decreased adiponectin are two major actors in the process called lipotoxicity related to an ectopic accumulation of TG associated with insulin resistance [11]. The mechanisms postulated for lipotoxicity imply the increased level of fatty acid derivatives, acyl-CoA, diglycerides, ceramides, present in the cytosol of some tissues such as...