- 198 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
New Insights in Intracerebral Hemorrhage
About This Book
The age-standardized mortality rate for hemorrhagic stroke has decreased worldwide over the past two decades, but incidence, number of deaths, and lost disability-adjusted life-years (DALY) continue to increase. Moreover, hemorrhagic stroke occurs half as frequently globally as ischemic stroke, but causes significantly more deaths and lost DALY. Milestone studies of the past decade - STICH, FAST, and INTERACT2 - indicate the importance of hyperacute care for intracerebral hemorrhage; despite this, there is to date no established strategy for patients analogous to reperfusion therapy for ischemic stroke. This book, written by world-renowned experts, covers all current topics related to the diagnosis and management of intracerebral hemorrhage. It will contribute to an improved understanding of current and future aspects concerning optimal management of patients. This is a comprehensive, up-to-date resource for neurologists, neurosurgeons and trainees.
Frequently asked questions
Information
Front Neurol Neurosci. Basel, Karger, 2016, vol 37, pp 107-129 (DOI: 10.1159/000437117)
Ultra-Early Hemostatic Therapy for Intracerebral Hemorrhage: Future Directions
Abstract
Scope of the Problem: Hematoma Growth
1. | Shorter time from symptom onset to first CT [12, 15, 21, 26, 38, 51, 62, 133] |
2. | Large hematoma size [30, 51, 62, 133]; hematoma volume on first CT<25 mm3 [26] |
3. | Irregular hematoma shape and heterogeneous lesions [12, 134] |
4. | MAP >120 mm Hg [30]; SBP ≥200 mm Hg [26]; highest SBP [135, 136]; history of hypertension [38] |
5. | GCS score ≤8 [30]; presence of consciousness disturbance [12]; higher NIHSS score [21] |
6. | History of cerebral infarction [26] |
7. | Liver disease [26] |
8. | Fasting plasma glucose ≥141 mg/dl and hemoglobin A1c ≥5.1% [26]; hyperglycemia [62, 133, 137] |
9. | Hypocholesterolemia [137] or hypercholesteremia [133] |
10. | Alcohol consumption (46.3 g/day) [12] |
11. | Reduced fibrinogen level (<87 mg/dl) [12]; elevated serum fibrinogen level (>523 mg/dl) [135] |
12. | Body temperature >37.5°C [135] |
13. | Neutrophil count (by 1,000-unit increase) [135] |
14. | IVH [135] |
15. | Admission cellular fibronectin level >6 μg/ml and admission interleukin-6 level >24 pg/ml [138] |
16. | Oral anticoagulation [15, 21, 23, 38, 51]; increased INR 2 h after presentation [22]; INR >2 before treatment or ≥24 h after PCC administration [24] |
17. | Use of antithrombotic agents prior to hemorrhage [21, 133] |
18. | Baseline weight [133] |
19. | Increased serum creatinine [133] |
20. | White-matter hyperintensities on MRI [139] |
CT = Computed tomography; MAP = mean arterial blood pressure; SBP = systolic blood pressure; GCS = Glasgow Coma Scale; NIHSS = National Institutes of Health Stroke Scale; IVH = intraventricular hemorrhage; INR = international normalized ratio; PCC = prothrombin complex concentrate; MRI = magnetic resonance imaging. | |
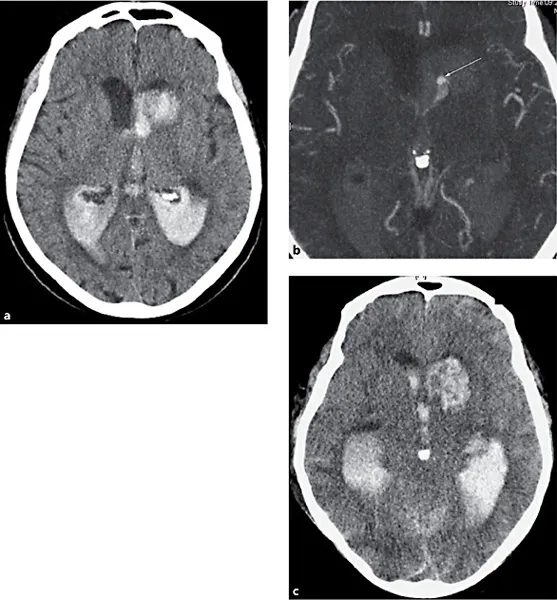
Prediction of Intracerebral Hemorrhage Growth: The Spot Sign
Table of contents
- Cover Page
- Front Matter
- Epidemiology of Intracerebral Haemorrhage
- Emergency Imaging of Intracerebral Haemorrhage
- Evidence-Based Critical Care of Intracerebral Hemorrhage: An Overview
- New Insights into Blood Pressure Control for Intracerebral Haemorrhage
- Emergency Reversal Strategies for Anticoagulation and Platelet Disorders
- Reperfusion-Related Intracerebral Hemorrhage
- Cerebral Microbleeds: Detection, Associations and Clinical Implications
- New Insights into Nonvitamin K Antagonist Oral Anticoagulants’ Reversal of Intracerebral Hemorrhage
- Ultra-Early Hemostatic Therapy for Intracerebral Hemorrhage: Future Directions
- Ventriculostomy and Lytic Therapy for Intracerebral Hemorrhage
- Surgical Craniotomy for Intracerebral Haemorrhage
- New Insights in Minimally Invasive Surgery for Intracerebral Hemorrhage
- Surgical Strategies for Acutely Ruptured Arteriovenous Malformations
- Prognosis and Outcome of Intracerebral Haemorrhage
- Author Index
- Subject Index