Clinical Handbook In Adolescent Medicine, A: A Guide For Health Professionals Who Work With Adolescents And Young Adults
A Guide for Health Professionals Who Work with Adolescents and Young Adults
- 780 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Clinical Handbook In Adolescent Medicine, A: A Guide For Health Professionals Who Work With Adolescents And Young Adults
A Guide for Health Professionals Who Work with Adolescents and Young Adults
About This Book
This clinical handbook is a valuable resource for any health professional who works with adolescents and young adults, whether in paediatric or adult acute care facilities or in the community. As a handbook it provides ready access to practical, clinically relevant and youth specific information.
This clinical handbook fills a clear gap, as most adolescent texts are primarily directed at paediatricians. This handbook extends its scope beyond paediatrics for three important reasons. First, many adolescents are managed by adult trained clinicians who have not had much exposure to or training in adolescent health. Secondly, the important health conditions of adolescents are often the important health conditions in young adults. Thirdly, with increased survival rates in chronic illness over the last two to three decades, it is becoming essential that clinicians in adult health care are able to assess and manage conditions that have their origins in childhood.
Each chapter is written by an expert in their field with a highly practical approach. The information is relevant and straightforward, with the aim of enhancing clinical skills.
Contents:
- Normal Physical Development and Growth at Puberty (Geoffrey Ambler)
- The Normal Development of the Adolescent Brain (Donna M Palmer and Leanne M Williams)
- Normal Psychosocial Development in Adolescence (David Bennett and Richard G MacKenzie)
- Body Image Issues in Adolescents (Jennifer O'Dea)
- Communicating with Adolescents (Richard G MacKenzie)
- Consent and Confidentiality (Michelle Yeo)
- Communicating with Parents and Carers (Anne Honey and Gwynneth Llewellyn)
- Communicating Electronically with Adolescents (Fiona Robards and Andrew Campbell)
- Education Issues (Margaret Allan)
- Adolescents and Young Adults in Adult Hospitals (Gail Anderson, Tegan Sturrock and Patricia Kasengele)
- Self-Management in Chronic Illness; Promoting Therapy Adherence (Michele Casey and Kate Steinbeck)
- Complex Medicopsychosocial Conditions: Chronic and Functional Disorders (Susan J Towns and Helen E Bibby)
- Transition from Paediatric to Adult Care in Chronic Illness (Sandra Whitehouse, Lynne Brodie and Susan J Towns)
- Resilience (Emily Klineberg)
- Alcohol and Other Drugs (Bronwyn Milne, Yvonne Bonomo and Gilbert Whitton)
- Unintentional Injuries Among Adolescents and Young Adults (Richard E Bélanger and Joan-Carles Suris)
- Rural and Remote Australian Adolescent Health Issues (Catherine Hawke)
- Important Medical and Mental Health Issues for Incarcerated and Homeless Youth (Stephen Stathis, Lee Hudson and Andrew Kennedy)
- The Dying Adolescent (Michael Stevens, Julie Dunsmore and John Collins)
- Disorders of Puberty (Ann Maguire and Kate Steinbeck)
- The Deaf Adolescent (Eric Weiselberg)
- The Adolescent and Young Adult with Intellectual Disability and Complex Health Needs (Helen Somerville and Cameron Ly)
- Key Issues in Adolescent Obesity (Shirley Alexander, Alison G Hoppin and Louise A Baur)
- Adolescents with Eating Disorders (Jorge L Pinzon, Gail Anderson and Simon Clarke)
- Adolescent Sexuality, Sexual and Reproductive Health (Melissa Kang, Rachel Skinner and Deborah Bateson)
- Physical Activity and Sports Medicine (Carolyn Broderick and Damien McKay)
- Depression and Anxiety (Sloane Madden)
- Assessment and Treatment of Psychotic Disorders in Adolescence (Jean Starling and Anthony Harris)
- Suicide and Self-Harm (Philip Hazell)
- Mental Health in Young People with Intellectual Disability and Autism (David Dossetor and Rameswaran Vannitamby)
- Sleep and Sleep Disorders in Adolescents (Karen Waters)
- Attention Deficit Hyperactivity Disorder (Michael R Kohn and Deborah Erickson)
- Immunisation and Infectious Diseases (Melina Georgousakis, Alexa Deirig and Robert Booy)
- Respiratory Disorders in Adolescence (Donald Payne and Siobhain Mulrennan)
- Common Adolescent Endocrine Disorders (Shubha Srinivasan)
- Diabetes During Adolescence (Kristine Heels, Nuala Harkin and Kim C Donaghue)
- Adolescent Bone Health (Craig Munns)
- Common Neurological Disorders (Richard Webster)
- Common Gastrointestinal Disorders of Adolescence (Annabel Magoffin)
- Common Dermatological Problems in Adolescents (Anuja Elizabeth George)
- Common Haematological Conditions in Adolescence (Julie Curtin)
- Allergic and Immunological Disorders in Adolescence (Alyson Kakakios, Dianne Campbell, Paul Turner and John Tan)
- Cancer in Adolescents and Young Adults (Bhavna Padhye and Melissa Gabriel)
- Late Effects of Childhood Cancer Therapy (Helena Gleeson)
- Common Cardiology Problems in Adolescence (Mugur Nicloae and Dorothy Radford)
- Adolescent Renal Medicine (Siah Kim and Deirdre Hahn)
- Common Rheumatological Conditions in Adolescence (Davinder Singh-Grewal)
- Genetics and Adolescents (David Sillence)
- Urological Problems in Adolescence (Grahame H H Smith)
- Common Gynaecological Problems in Adolescence (Kim Matthews and Peter Benny)
- The Andrology of Adolescence (David J Handelsman)
- Cardiovascular Risk Factors and Atherosclerosis (Marc S Jacobson and Michael R Kohn)
Readership: Clinicians, nurses, doctors and all other professionals in healthcare.
Frequently asked questions
Information
Chapter 1
Normal Physical Development and Growth at Puberty
Geoffrey Ambler
1. Introduction
- Thelarche — the onset of breast development in girls.
- Pubarche — the onset of sexual hair development in boys or girls.
- Menarche — the onset of the first menstrual period in girls.
- Gonadarche — the onset of mature gonadal function (sperm production in boys or ovulation in girls).
- Adrenarche — the onset of adrenal androgen production in boys or girls.
2. The Physiology of Puberty
2.1. Activation of the Hypothalamic–Pituitary–Gonadal Axis
2.2. Adrenarche
2.3. The Growth Hormone Axis
3. Timing of Puberty and Secular Trends
4. Physical Changes of Puberty
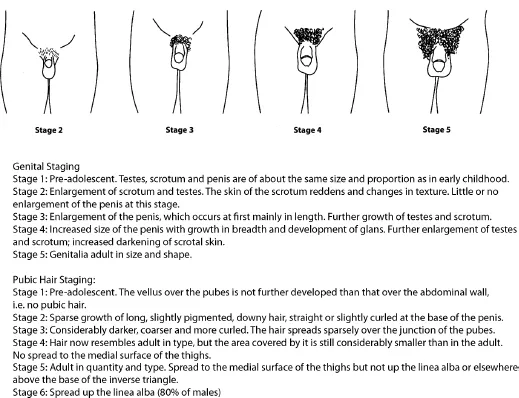
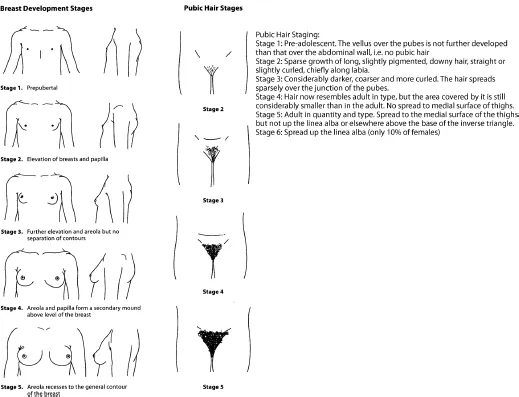
4.1. Physical Changes in Boys (see Fig. 1 and Table 1)
Table of contents
- Cover
- A Clinical Handbook in Adolescent Medicine
- Title Page
- Copyrights
- Contents
- Foreword
- Acknowledgements
- Contributors
- Chapter 1: Normal Physical Development and Growth at Puberty
- Chapter 2: The Normal Development of the Adolescent Brain
- Chapter 3: Normal Psychosocial Development in Adolescence
- Chapter 4: Body Image Issues in Adolescents
- Chapter 5: Communicating with Adolescents
- Chapter 6: Consent and Confidentiality
- Chapter 7: Communicating with Parents and Carers
- Chapter 8: Communicating Electronically with Adolescents
- Chapter 9: Education Issues
- Chapter 10: Adolescents and Young Adults in Adult Hospitals
- Chapter 11: Self-Management in Chronic Illness; Promoting Therapy Adherence
- Chapter 12: Complex Medicopsychosocial Conditions: Chronic and Functional Disorders
- Chapter 13: Transition from Paediatric to Adult Care in Chronic Illness
- Chapter 14: Resilience
- Chapter 15: Alcohol and Other Drugs
- Chapter 16: Unintentional Injuries Among Adolescents and Young Adults
- Chapter 17: Rural and Remote Australian Adolescent Health Issues
- Chapter 18: Important Medical and Mental Health Issues for Incarcerated and Homeless Youth
- Chapter 19: The Dying Adolescent
- Chapter 20: Disorders of Puberty
- Chapter 21: The Deaf Adolescent
- Chapter 22: The Adolescent and Young Adult with Intellectual Disability and Complex Health Needs
- Chapter 23: Key Issues in Adolescent Obesity
- Chapter 24: Adolescents with Eating Disorders
- Chapter 25: Adolescent Sexuality, Sexual and Reproductive Health
- Chapter 26: Physical Activity and Sports Medicine
- Chapter 27: Depression and Anxiety
- Chapter 28: Assessment and Treatment of Psychotic Disorders in Adolescence
- Chapter 29: Suicide and Self-Harm
- Chapter 30: Mental Health in Young People with Intellectual Disability and Autism
- Chapter 31: Sleep and Sleep Disorders in Adolescents
- Chapter 32: Attention Deficit Hyperactivity Disorder
- Chapter 33: Immunisation and Infectious Diseases
- Chapter 34: Respiratory Disorders in Adolescence
- Chapter 35: Common Adolescent Endocrine Disorders
- Chapter 36: Diabetes During Adolescence
- Chapter 37: Adolescent Bone Health
- Chapter 38: Common Neurological Disorders
- Chapter 39: Common Gastrointestinal Disorders of Adolescence
- Chapter 40: Common Dermatological Problems in Adolescents
- Chapter 41: Common Haematological Conditions in Adolescence
- Chapter 42: Allergic and Immunological Disorders in Adolescence
- Chapter 43: Cancer in Adolescents and Young Adults
- Chapter 44: Late Effects of Childhood Cancer Therapy
- Chapter 45: Common Cardiology Problems in Adolescence
- Chapter 46: Adolescent Renal Medicine
- Chapter 47: Common Rheumatological Conditions in Adolescence
- Chapter 48: Genetics and Adolescents
- Chapter 49: Urological Problems in Adolescence
- Chapter 50: Common Gynaecological Problems in Adolescence
- Chapter 51: The Andrology of Adolescence
- Chapter 52: Cardiovascular Risk Factors and Atherosclerosis
- Abbrevations
- Index