eBook - ePub
Contemporary Surgical Management of Liver, Biliary Tract, and Pancreatic Disease
This is a test
- 672 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Contemporary Surgical Management of Liver, Biliary Tract, and Pancreatic Disease
Book details
Book preview
Table of contents
Citations
About This Book
Contemporary Surgical Management of Liver, Biliary Tract, and Pancreatic Diseases presents an excellent resource for surgical residents, hepatobiliary fellows and practicing surgeons interested in hepatobiliary surgery. This textbook offers a readable, concise and practical alternative. It is divided into three sections: liver, biliary tract, and pancreatic diseases. Each section covers the spectrum of benign and malignant disease. In addition, several chapters in each section are devoted to surgical techniques. This textbook should ultimately serve as an essential source for the rapidly evolving field of hepatobiliary surgery and its practitioners.
Contents:
- Liver Disease:
- Liver Anatomy and Anatomic Variants (Shuja Ahmed and Janet E Tuttle-Newhall)
- Imaging of the Liver (Nestor Villamizar Ortiz and Bryan M Clary)
- Hepatic Abscess (Georgia Beasley and Dan G Blazer III)
- Cystic Disease of the Liver (Marcus Darrabie and Carlos E Marroquin)
- Benign Liver Lesions (Immanuel Turner and Paul C Kuo)
- Primary Hepatic Malignancies (Andrew S Barbas and Rebekah R White)
- Surgical Treatment of Hepatic Metastases (Nicole de Rosa, Dan G Blazer III and Bryan M Clary)
- Cirrhosis and Portal Hypertension (Keshava Rajagopal and Carlos E Marroquin)
- Technical Management of Ascites (Carlos E Marroquin and Bridget M Marroquin)
- Variceal Therapies (Carlos E Marroquin)
- Liver Failure (Valentino Piacentino, Deborah L Sudan and Janet E Tuttle-Newhall)
- Liver Transplantation (Katia Papalezova, Carlos E Marroquin, Bradley H Collins, Janet E Tuttle-Newhall and Paul C Kuo)
- Embolization of Liver Tumors (Leo Villegas and Paul V Suhocki)
- Radiofrequency Ablation (Syamal Bhattacharya and Carlos E Marroquin)
- Regional Therapies for Hepatic Malignancy (Lindsay Talbot and Dan G Blazer III)
- Hepatic Resection (Michael E Barfield and Bryan M Clary)
- Surgical Techniques: Liver Procurement and Transplantation (Deepak Vikraman and Carlos E Marroquin)
- Biliary Disease:
- Biliary Anatomy (Asvin Ganapathi and Sandhya A Lagoo-Deenadayalan)
- Imaging of the Biliary Tree (Asad A Shah and Theodore N Pappas)
- Benign Gallbladder Disease: Cholelithiasis, Polyps, Gallstone Ileus (Kelley Hutcheson and Dan G Blazer III)
- Benign Gallbladder Disease: Cholecystitis (Ryan Turley, Kelley Hutcheson and Lisa Pickett)
- Benign Gallbladder Disease: Bile Duct Injuries (Dawn M Elfenbein and Mark Shapiro)
- Benign Gallbladder Disease: Postcholecystectomy Syndrome and stricture (Judson B Williams and Sandhya A Lagoo-Deenadayalan)
- Benign Gallbladder Disease: Choledocholithiasis and Cholangitis (Loretta Erhunmwunsee and Aurora D Pryor)
- Gallbladder Cancer (Asad A Shah, Srinevas K Reddy, Dan G Blazer III and Bryan M Clary)
- Choledochal Cysts (Brian R Untch and Abigail E Martin)
- Primary Biliary Cirrhosis and Primary Sclerosing Cholangitis (Vanessa Teaberry and Alastair Smith)
- Bile Duct Cancer: Peripheral and Hilar Cholangiocarcinoma (Melissa Danko and Dana Portenier)
- Interventional Biliary Techniques (Nicholas D Andersen and Paul V Suhocki)
- Surgical Techniques: Lap/Open Cholecystectomy (Sean Lee and Aurora D Pryor)
- Surgical Techniques: Bile Duct Injury Repair (Sapan Desai and Dan G Blazer III)
- Surgical Techniques: Common Bile Duct Exploration (Sebastian G de la Fuente, Aurora D Pryor and Theodore N Pappas)
- Surgical Techniques: Bile Duct Resection/Reconstruction (Sarah Evans and Carlos E Marroquin)
- Surgical Techniques: Transduodenal Techniques (Sean Lee and Katia Papalezova)
- Diseases of the Pancreas:
- Pancreas Anatomy and Anatomic Variants (Mani A Daneshmand and Eugene P Ceppa)
- Imaging of the Pancreas (Kristy Rialon, Courtney Coursey and Rendon C Nelson)
- Acute Pancreatitis (Mayur B Patel and Theodore N Pappas)
- Chronic Pancreatitis (Jack Haney and Eugene P Ceppa)
- Cystic Neoplasms of the Pancreas (Eugene P Ceppa and Douglas S Tyler)
- Periampullary Cancer (Diana L Diesen and Theodore N Pappas)
- Pancreatic Neuroendocrine Tumors (Tamarah Westmoreland and John Olson)
- Unusual Pancreatic Neoplasms (James Padussis and Douglas S Tyler)
- Pancreas and Islet Cell Transplantation (Keri E Lunsford and Bradley H Collins)
- Interventional Techniques (Stephen Philcox and Paul Jowell)
- Surgical Techniques: Whipple (Rebekah R White and Eugene P Ceppa)
- Surgical Techniques: Palliative Surgery (Jeffrey Nienaber and Theodore N Pappas)
- Surgical Techniques: Distal Pancreatectomy (Jin S Yoo and Aurora D Pryor)
- Surgical Techniques: Enucleation Procedures and Central Pancreatectomy (Elisabeth Tracy and Theodore N Pappas)
- Surgical Techniques: Chronic Pancreatic Procedures (John C Haney and Eugene P Ceppa)
- Surgical Techniques: Pancreas Transplantation (Errol L Bush, Kadiyala V Ravindra and Bradley H Collins)
Readership: Medical students, resident trainees, nurses and physician assistants.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Contemporary Surgical Management of Liver, Biliary Tract, and Pancreatic Disease by Dan G Blazer III, Paul C Kuo, Theodore Pappas, Bryan M Clary in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
Topic
MedicineSection 1:
Liver Disease
| LIVER ANATOMY AND ANATOMIC VARIANTS | 1 |
INTRODUCTION
From the first liver resection by A. Luis in 18861 to modern day liver transplantation, hepatobiliary surgery has witnessed major advancements over the last century. Much of this technical achievement has been attained on the back of progressively improved understanding of the liver anatomy and its potential variant. From Cantlie to Couinaud, many anatomists contributed towards this modern-day understanding of the liver anatomy. The liver, by virtue of its friability and propensity to bleed from rich vascularization, continues to be a surgical challenge for today’s surgeon despite access to modern instruments and equipment. Good working knowledge of the hepatic anatomy with its variants is therefore an important prerequisite to successful hepatobiliary surgery and the only way to minimize associated complications.
This chapter reviews the anatomy of the liver in some detail. All functional components of the liver, including arterial supply, venous outflow, biliary tree and lymphatics, are sequentially reviewed.
FUNCTIONAL SURGICAL ANATOMY
The functional anatomy of the liver has been a subject of much debate and research over the last century and even till today among surgical scholars. The internal liver structure has been clarified.2–4,5–8 This “functional anatomy” describes liver architecture in terms of hepatic segments based on the distribution of portal pedicle and location of hepatic veins. Essentially, the three main hepatic veins divide the liver into four sectors, each of which receives a portal pedicle with an alternating arrangement of hepatic vein and portal pedicle.
According to Couinaud’s landmark description,7 the liver parenchyma overlying the hepatic veins is termed a scissura. Thus, the main portal scissura (better known as Cantlie’s line) contains the middle hepatic vein and extends from the middle of the gallbladder anteriorly to the left of the vena cava posteriorly. This imaginary line divides the liver into right and left lobes and has been used by surgeons to delineate the lobes as such. Of clinical significance, the left and right lobes of the liver are independent in terms of portal and arterial vascularization and of biliary drainage. This anatomical divide is important in determining types and extent of resections.
Subsequently, the right and left lobes are further subdivided into two sectors each by two other portal scissurae. The right portal scissura divides the right lobe into anteromedial and posterolateral sectors. The right hepatic vein runs in the right scissura. Each of these sectors is further subdivided into segments. The anteromedial sector contains segment V anteriorly and segment VIII posteriorly. The posterolateral sector contains segment VI anteriorly and segment VII posteriorly. The left portal scissura containing the left hepatic vein divides the left lobe into anterior and posterior sectors. Of note, the left portal scissura is not within the umbilical fissure but located posterior to the ligamentum teres. The umbilical fissure overlies a portal pedicle and thus divides the anterior sector into segment III and IV (quadrate lobe). The posterior sector is only composed of segment II.
The caudate lobe is referred to as segment I. It lies posteriorly in close proximity to the inferior vena cava and segment IV. Functionally, it is an autonomous segment as it receives its blood supply from both the right and left branches of the hepatic artery and portal vein. Also, its venous drainage is directly into the inferior vena cava instead of the hepatic vein. This is important in setting of Budd-Chiari syndrome. Obstructed hepatic veins cause hepatic outflow to be directed through a hypertrophied caudate lobe into the inferior vena cava.
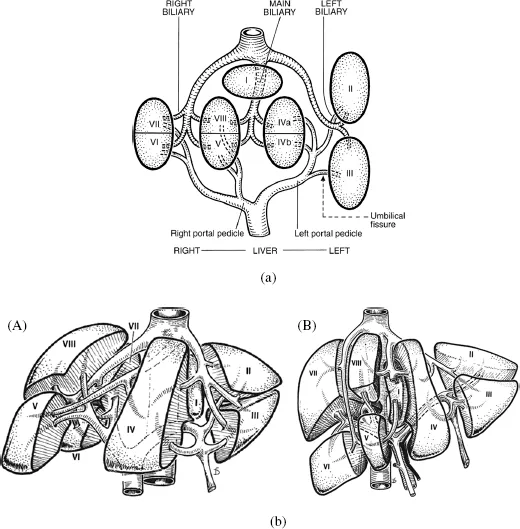
Figure 1. Schematic representation of functional anatomy of liver. Used with permission from Surgery of the liver, biliary tract and pancreas. Volume 1. (4th Edition) LH Blumgart.
CLINICAL SIGNIFICANCE
Knowledge of the functional anatomy is important to undertake various types of partial hepatectomies such as lobectomy, and segmentectomies. Understanding the anatomy is less important when planning wedge or “nonanatomic” liver resections. Good working knowledge of the vasculature and bile ducts allows accurate resection with a lower chance of biliary complications, including leaks. Knowledge of the anatomy can also ensure that the post-resected liver remains viable with normal arterial inflow and venous outflow to allow prompt regeneration.
LIVER BLOOD SUPPLY
The liver normally receives 25% of the total cardiac output and is unique in that it receives its blood supply from two main sources: the hepatic artery and portal vein. The hepatic artery provides about 25% of the hepatic blood flow and 50% of the oxygen supply. The portal vein contributes about 75% of the blood flow and 50% of oxygen supply. Mixing of the arterial portal blood occurs in the sinusoids which are drained by the hepatic veins into the inferior vena cava (IVC).
HEPATIC ARTERY
The anatomy of the hepatic artery and its variants has been described in the literature.9–13 The arterial patterns are of importance in planning and performance of all hepatic surgeries.
Aberrant hepatic arteries are found in 45% of population, based on postmortem examinations. An aberrant artery is accessory if it supplies a segment of the liver that also receives blood supply from a normal hepatic artery. It is a replacing artery if it is the only blood supply to such lobe or segment.
The common hepatic artery originates from the celiac trunk in 86% of the population. Other sources are superior mesenteric artery (2.9%), aorta (1.1%) and, very rarely, left gastric artery.14 After its origin, the common hepatic artery runs horizontally along the upper border of the head of the pancreas and gives off the gastroduodenal (GDA) artery posterior and superior to the duodenum. The supraduodenal artery and right gastric artery originate just distal to the GDA. The continuation of the hepatic artery beyond the origins of these vessels is known as the hepatic artery proper (HAP). It turns upwards to ascend in the lesser omentum, enveloped by the hepatoduodenal ligament, in front of the epiploic foramen of Winslow. Within the hepatoduodenal ligament, the HAP lies to the left of the common bile duct and anterior to the portal vein. Together, the hepatic artery proper, the common bile duct and the portal vein form the portal triad. Within the ligament, the hepatic artery proper divides into right and left hepatic arteries.
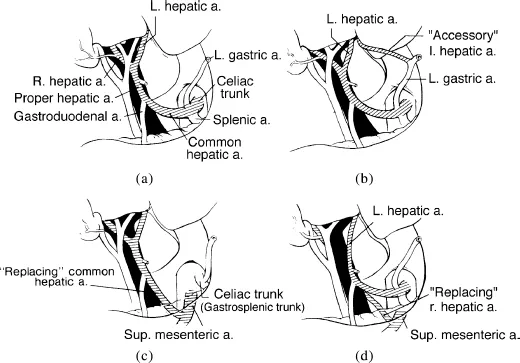
Figure 2. (A) Normal hepatic artery from celiac trunk. (B) Accessory left hepatic artery from left gastric artery. (C) Replacing common hepatic artery arising from superior mesenteric artery. (D) Replacing right hepatic artery arising from superior mesenteric artery. Hepatic Surgical Anatomy. Surg Clin N Am 84 (2004) 413–415; used with permission.
The right hepatic artery is a branch of the hepatic artery proper in the majority of the population; however, in 17% of subjects, it arises from the superior mesenteric artery.14 A “replaced” right hepatic artery is more common than an “accessory” right hepatic artery. Inadvertent ligation of a replaced right hepatic artery, especially where it crosses the junction of the cystic duct and common bile duct, during cholecystectomy, deprives blood supply to the right lobe of the liver and can lead to significant complications. In contrast, ligation of an accessory right hepatic artery that derives from superior mesenteric artery has less significant consequences. At the porta hepatis, the right hepatic artery normally passes to the right behind the hepatic duct and anterior to the portal vein to enter the Calot triangle formed by the cystic duct, the hepatic duct and the liver. In 15% of individuals, however, it may pass anterior to the hepatic duct. This variation is worth remembering during exploration of the common bile duct or routine cholycystectomies.
Before entering the liver, the right hepatic artery gives off the cystic artery. Within the liver, the right hepatic artery divides into anterior and posterior segmental arteries which divide further into superior and inferior arteries to supply the respective subsegments. An artery for the caudate lobe also originates and supplies the caudate process and the right side of the caudate lobe. These arteries are found under the respective bile duct branches.
The left hepatic artery usually originates from the HAP. An aberrant left hepatic artery originating from the left gastric artery occurs in 30% of patients.15 In this variant form, the left hepatic artery is a replaced versus accessory artery in a ratio of 1:1. If replaced, only the right hepatic artery comes off from the celiac axis, whereas, in the presence of an accessory vessel, the common hepatic artery takes its usual course and supplies a right and a left hepatic artery. Ligation of a replaced left hepatic artery, such as during gastrectomy or laparoscopic Nissen fundoplication, would compromise the blood supply to the left lobe of liver. In addition, an accessory left hepatic artery may also come from the right hepatic artery.
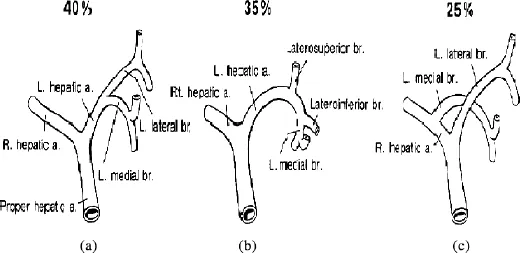
Figure 3. Variations in branching of left hepatic artery. (A) Bifurcation into medial and lateral segmental arteries. (B) Division of lateral segmental artery into laterosuperior and lateroinferior branches. (C) The left medial segmental artery arises from right hepatic artery. Hepatic Surgical Anatomy. Surg Clin N Am 84 (2004) 413–415; used with permission.
After its origin, the left hepatic artery supplies the entire left lobe of liver in 40% of patients by dividing into medial and lateral segmental arteries. Interestingly, in 25% of patients, the left hepatic artery supplies only the left lateral segmental; the left medial segment being supplied by a branch of the right hepatic artery crossing the midline. The left hepatic artery also gives off a branch for the caudate lobe supplying its left side.
PORTAL VEIN
The portal vein forms behind the head of the pancreas at the level of L2 through a confluence of the superior mesenteric and splenic veins. It runs behind the first portion of the duodenum and then along the right border of the lesser omentum — as part of portal triad — for a length of 8–10 cm. In its upward course, the portal vein receives the coronary vein, which is a continuation the left gastric vein and the esophageal venous plexus. At the liver hilum, it divides into right and left branches to the respective lobes.
The right branch of the portal vein is shorter of the two branches and is located anterior to the caudate process. Near its origin, it gives off a branch for the caudate lobe and then divides into anterior and posterior segmental branches, which further subdivide into superior and inferior subsegmental branches for respective parenchymal subsegments.
The left portal vein is smaller and longer than its counterpart. It also gives off a caudate lobe branch at its origin following which it divides into medial and lateral branches. The medial vessel contains a dilatation, the pars umbilicus, which represents the orifice of the obliterated embryonic ductus venosus.
Portal Vein Variations and Ano...
Table of contents
- Cover
- Half Title
- Title
- Copyrights
- CONTENTS
- Contributing Authors
- Section 1 Liver Disease
- Section 2 Biliary Disease
- Section 3 Diseases of the Pancreas
- Index