![]()
1
INTRODUCTION
Age-related macular degeneration is the commonest cause of visual impairment registration in the UK. Intravitreal injections (injections into the vitreous gel of the eye) of antivascular endothelial growth factors (anti-VEGF’s) such as Lucentis® (ranibizumab), Avastin® (bevacizumab) and Eylea® (aflibercept) are now widely accepted to reduce the progression of “wet” macular degeneration. There is also good evidence of their efficacy in macular oedema secondary to diabetes and vein occlusions.
Ophthalmic nurse practitioners and allied health professionals are increasingly becoming invaluable team members for delivering intravitreal injections, particularly as the clinical demand grows. We have written this handbook to aid our colleagues in such an endeavour and hope that it will provide concise, relevant information in a format that is easy to carry around and access. Towards the end we have outlined our experience in designing a training structure and it is our sincere hope that this will provide a framework for others too. We have extensive experience in organising wetlab sessions for both ophthalmic trainees and nurse practitioners, and have added some easy tips for readers to set up a session of their own. The appendices contain the latest information on basic life support and anaphylaxis treatment. Whilst the practitioner will always be in a well-supported environment and emergency response teams will be just a phone call away, it is beneficial to be familiar with these algorithms. The book is aimed primarily at nurse practitioners and allied health professionals, but we are confident that it will also be a useful reference for junior ophthalmic trainees learning how to perform intravitreal injections.
We wish you all the best for your career as part of the retinal team!
Salman Waqar
Jonathan Park
![]()
2
BASICS
In order to be proficient in intravitreal injections, it is crucial to appreciate the structure of the eye and how this knowledge can be used to give a safe injection.
The eye is a highly specialised organ of photoreception. This is a process by which light energy from the environment produces changes in specialised nerve cells in the retina (rods and cones). These changes result in action potentials (the electrical voltage across a cell) that are subsequently relayed to the optic nerve and then to the brain, where the information is processed and consciously appreciated as vision.
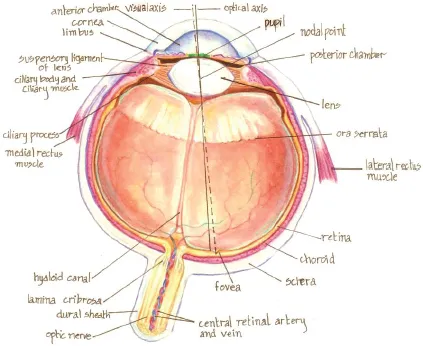
The eye is an approximate sphere 2.5 cm in diameter (equivalent to an axial length of 25 mm), with a volume of 5 mL (fills 1/6 of the orbit, whose volume is 30 mL). It consists of three basic layers.
THE THREE LAYERS OF THE EYE
1.The fibrous corneoscleral coat consists of the cornea and the sclera.
•The Cornea
This is the anteriormost, transparent window of the eye. The cornea meets the sclera at the limbus, which is also where the conjunctiva ends. The conjunctiva covers the sclera but not the cornea. The cornea is kept transparent by its avascularity and the innermost monolayer of cells (endothelium), which pumps fluid out of the corneal stroma. It presents a tough barrier to trauma and infection, and is responsible for about 2/3 of the eyes’ refractive power (the remaining 1/3 comes from the lens).
Fig. 2.1. The eye in cross section.
•The Sclera
This is an opaque white fibrous coat that also protects the eye and maintains its shape owing to inherent structural integrity.
2.The uvea (or uveal tract) is the middle vascular pigmented layer of the eye and consists of the iris, ciliary body and choroid.
•The Iris
This is a thin contractile circular disc, analogous to the diaphragm of a camera. The iris separates the anterior and posterior chambers, which are filled with aqueous humour and are in continuity through an opening, the pupil. The iris is attached by its root at the “angle” (iridocorneal) of the anterior chamber where it merges with the ciliary body and trabecular meshwork. Aqueous humour drains mainly through the trabecular meshwork, which is visible using a mirror within a contact lens called a gonioscope.
•The Ciliary Body
This is approximately 6 mm in width and is responsible for the production of aqueous humour. It also contains muscles, which are attached to the zonular ligaments of the lens (changing its shape on contraction to focus or accommodate). It has two parts: the pars plicata and the pars plana. The pars plicata is the anterior part. It is 2 mm long (measured from the limbus) and contains about 70 ciliary processes which are the site of attachment for the aforementioned zonular ligaments The pars plana is a posterior flat area 4 mm long. As the sclera and cornea are relatively rigid, excess production or reduced drainage of aqueous humour or injection of substances into the eye leads to raised intraocular pressure (normally this is up to 21 mmHg). Intraocular pressure is high immediately after intravitreal injections (it can be as high as 60 mmHg). Normalisation of the pressure usually occurs over 30 min after injection and is dependent on aqueous humour outflow through the trabecular meshwork. The safest site for administering intravitreal injections is through the pars plana. This is because it lies behind the lens and in front of the retina, thus avoiding damage to either of these structures.
•The Choroid
This highly pigmented and vascular posterior portion lies between the sclera and the retina, and extends forwards to the ciliary body. Its principal function is to nourish the outer layers of the retina and prevent unwanted light from reflecting back through the retina. It is composed of an outer layer of large-calibre blood vessels, which divide into smaller-diameter vessels and ultimately form the choriocapillaris (a network of capillaries). These drain into the vortex veins, which ultimately drain into the superior and inferior ophthalmic veins. The innermost layer of the choroid is a membrane called Bruch’s membrane. The basal portion of the retinal pigment epithelium is attached to this membrane. This is of clinical importance, as in age-related macular degeneration it is Bruch’s membrane that is breached by abnormal choroidal blood vessels, leading to pathognomic features of the disease (as will be discussed later, in the imaging section).
3.The retina (neural layer) is where photoreception occurs. It consists of two primary layers: the inner neurosensory retina and an outer layer called the retinal pigment epithelium (RPE). Anatomically it comprises the following regions:
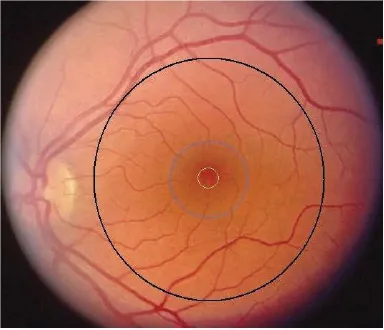
•The macula (Latin for “patch”; same as the macula lutea) is the area within the main vascular arcades and is 5–6 mm in diameter. Cone photoreceptors are mostly concentrated here for fine resolution (maximum density in the fovea).
•The fovea (Latin for “pit”) is the central 1.5-mm-diameter area of the macula. The foveola is the central 0.35-mm-diameter area of the fovea (Fig. 2.2).
•The optic disc is 1.5 mm in diameter. It contains no normal retinal layers or photoreceptors (thus causing the blind spot) and is the area where nerve fibres of retinal ganglion cells pierce the sclera to enter the optic nerve. The central pale thinned area of the disc forms the cup, which becomes progressively enlarged through loss of ganglion cells in glaucoma. The cup’s vertical diameter is measured in relation to the disc’s diameter when one is monitoring a patient with glaucoma (referred to as the cup-to-disc ratio).
•The peripheral retina is rich in rod photoreceptors which provide acuity at low levels of illumination.
•The ora serrata is where the peripheral retina ends. This is approximately 7 mm from the limbus.
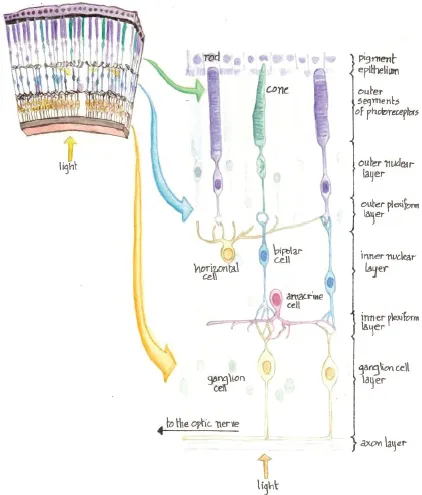
The Retina in Cross Section
The retina consists of 10 layers. From posterior to anterior these are (Fig. 2.3):
Fig. 2.2. A normal fundus photograph (left eye) showing the approximate locations of the macula (black circle), fovea (blue circle) and foveola (yellow circle).
1.Retinal pigment epithelium (RPE). This is a monolayer of cells which have several functions, including maintaining the adhesion of the neurosensory retina, rendering the sub-retinal space dry, removing shed portions of photoreceptor outer segments, contributing to the transport and storage of metabolites/vitamins and providing a blood retinal permeability barrier.
2.Photoreceptor layer. This contains rod and cone inner/outer segments. The outer segments contain the visual pigments that are responsible for absorption of light and initiation of the neuroelectrical impulse, whilst the inner segments contain the cellular apparatus required to provide energy, e.g. mitochondria. The junction of the two segments is visible on high resolution OCT, as discussed later.
3.External limiting membrane. This is a histological feature of the retina. It is a dark line caused by junctions between photoreceptors and Müller cells. It is located between the photoreceptor and outer nuclear layers.
Fig. 2.3. The retina in cross section.
4.Outer nuclear layer. This contains the nucleated cell bodies of the rods and cones. Cones subserve fine resolution essential for reading, spatial resolution and colour vision, whilst rods sense contrast, brightness and motion. Rods are also mainly responsible for peripheral and night vision.
5.Outer plexiform layer. This contains the cone and rod axons. It also contains dendrites of horizontal and bipolar cells.
6.Inner nuclear layer. This contains the nuclei of horizontal cells, bipolar cells, amacrine cells and Müller cells.
7.Inner plexiform layer. This contains the axons of bipolar cells and amacrine cells along with dendrites of ganglion cells.
8.Ganglion cell layer. This contains the nuclei of ganglion cells.
9.Nerve fibre layer (axon layer). This is formed by the axons of ganglion cells traversing the retina to leave the eye at the optic disc.
10.Inner limiting membrane. This is a membrane on the inner surface of the retina.
THE VITREOUS
The vitreous is a thick transparent substance that fills the centre of the eye between the lens and the retina. It is composed mainly of water and constitutes about 2/3 of the eye’s volume. The viscous properties of the vitreous allow the eye to return to its normal shape if compressed.
In children, the vitreous has a consistency similar to that of an ...