
Algorithms in Differential Diagnosis
How to Approach Common Presenting Complaints in Adult Patients, for Medical Students and Junior Doctors
- 500 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Algorithms in Differential Diagnosis
How to Approach Common Presenting Complaints in Adult Patients, for Medical Students and Junior Doctors
About This Book
This is a book for medical students and first-year doctors who wish to learn how to approach a patient's symptoms, and sharpen their skills of clinical reasoning and diagnosis.
Fifty-four presenting symptoms are discussed, covering approaches and conditions across various medical and surgical disciplines. Each chapter sets out the thought process behind history, examination, and investigations for a symptom, providing a systematic and practical algorithm to distinguish one differential from another. The reader will gain not only a functional approach to patients' presenting complaints, but also learn how to better organize and apply medical knowledge in diagnostic reasoning.
Contents:
- Introduction
- Heart and Lungs
- Gut and Abdomen
- Kidneys and Urinary Tract
- Brain, Nerves and Senses
- Blood
- Endocrine and General Physiological Disturbances
- Skin and Subcutaneous Tissues
- Joints and Muscles
- Female Genital Tract
Readership: Medical students and first-year doctors.Differential Diagnosis;Symptoms;History Taking;Clinical Reasoning;Medicine0 Key Features:
- This book covers common presenting complaints in adult patients, cutting across different clinical specialties — from internal medicine subspecialties, to surgical disciplines, orthopaedics, and gynaecology
- To help students and junior clinicians approach differential diagnosis with smart strategies. this book provides the basic schemata, which categorizes possible diagnoses in terms of their clinical picture, identifies key differentiators, and discusses the reasoning process how to comprehensively consider all possibilities yet narrow down to the most likely diagnosis
- Every chapter provides a clinical vignette, with a discussion on how the suggested algorithm can be applied to the clinical scenario
- The book is written with input from 15+ senior subspecialty experts
Frequently asked questions
Information
Chapter
22
An Approach to Headache
New Acute Headache
History and Examination
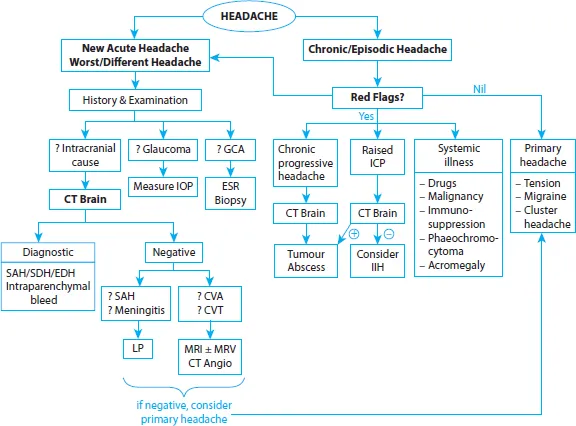
Referred pain: Two causes of referred pain require emergent treatment—these must be identified on history and examination, not CT brain. | Workup |
•Acute closed-angle glaucoma: Unilateral headache ± vomiting with severe eye pain, blurring of vision and halos around lights. Eye is red with a fixed, mid-dilated pupil. A relative afferent pupillary defect can be seen if the optic nerve is damaged. Urgent treatment prevents blindness. | –Measure intra-ocular pressure, for example, Goldmann tonometry |
•Giant cell arteritis (temporal arteritis): Unilateral headache with jaw claudication (jaw pain when chewing), transient visual loss or visual field defect and scalp tenderness. There may be systemic symptoms of polymyalgia rheumatica (joint pains, peripheral synovitis, constitutional symptoms). Examination may find visual field defect and optic disk swelling. This is an autoimmune disease usually in > 50 year olds; early treatment prevents visual loss. | –ESR: usually high –Confirmation via temporal artery biopsy (but do not wait to start treatment, and beware of a falsely normal biopsy due to skip lesions) |
Intracranial Causes: Upfront CT Brain
Further Investigation: (a) Suspect SAH or Meningitis
Table of contents
- Cover Page
- Title Page
- Copyright Page
- Contents
- Preface
- Subspecialty Reviewers
- Acknowledgements
- Introduction
- Heart and Lungs
- Gut and Abdomen
- Kidneys and Urinary Tract
- Brain, Nerves and Senses
- Blood
- Endocrine and General Physiological Disturbances
- Skin and Subcutaneous Tissues
- Joints and Muscles
- Female Genital Tract
- Index to Conditions