- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Equine Clinical Immunology
About this book
Equine Clinical Immunology offers comprehensive information on equine immunological disorders. • Provides a complete, equine-specific reference on clinical immunology
• Focuses on clinically relevant information for the diagnosis and treatment of horses with immune disorders
• Illustrates the concepts discussed using drawings, photographs, and tables
• Presents key concepts, clinical assessment information, and treatment approaches in text boxes for ease of use
• Offers a practical, clinically oriented approach ideal for equine specialists
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
1
The Immune System
M. Julia B. Felippe
1.1 Definition
The immune system is a network of cells and proteins that interact in tissues and organs to protect the body from infection, and also to promote healing. In general, immunity involves: the generation of inflammation; the removal and destruction of pathogens; the expansion of immune cell population and development of memory, specifically against the antigenic insult; control of inflammation; and tissue repair. The immune mechanisms aim to recognize and attack non-self molecules, although dysregulation can cause immunodeficiencies (e.g., insufficient protective response) or immune-mediated damage of self-molecules (i.e., autoimmune diseases and hypersensitivity reactions).
Classically defined, the immune system promotes immunity through innate and adapted segments. The innate immune cells and proteins provide immediate response and action against pathogens in a somewhat unspecific manner, while the adapted immune cells require priming with pathogen, cell co-stimulation and activation before function, and development of memory.
Immune cells cross-activate or cross-repress each other through cell-cell interactions, and in response to cytokines and chemokines, which are secreted proteins that function primarily in autocrine and paracrine manners and, sometimes, endocrine. Ligand-receptor or cytokine-cytokine receptor interactions lead to corresponding cell signaling, transcription and translation for immunostimulatory or immunosuppressive outcomes.
1.2 The organs of the immune system
The organs of the immune system are referred to as central (e.g., bone marrow and thymus), where cells are produced and go through initial or complete development; or peripheral (e.g., lymph nodes, spleen, and mucosa-associated lymphoid tissues (MALT), also known as bronchus-associated (BALT) and gut-associated (GALT) lymphoid tissues), in which cells complete their development and become activated upon encountering antigen.
Epithelial cells of the skin and mucosa comprise anatomical barriers to pathogens and toxins. Secretions (e.g., lysozymes in saliva and tears, low stomach pH) and clearance mechanisms (e.g., mucociliary system of the respiratory tract) add protection as physiological barriers. In addition, epithelial and endothelial cells can become activated by pathogens and secrete cytokines (e.g., interferon-beta, TNF-alpha), chemokines and selectins/integrins, which attract inflammatory cells. Damage to these structures and mechanisms decreases protection and favors pathogen invasion and replication.
Immune cells circulate through blood and lymph throughout the body, and migrate to tissues and lymphoid tissues, often attracted by chemokines; they can either settle and become resident cells, or constantly recirculate in search of an antigen or a site of inflammation. Cells circulating in the lymphatics re-enter the blood circulation via the thoracic duct and, from the blood, they can be attracted and migrate to tissues via diapedesis. From tissues, they can reach regional lymphoid structures and draining lymph nodes via draining lymphatics. Immune cells and antigens reach the spleen via blood, which works as a filter, with small capillary structures surrounded by organized lymphoid tissues.
Diapedesis is the process of extravasation of leukocytes from the blood stream into tissues. Sentinel cells of the immune system resident at tissue sites (e.g., macrophages, mast cells) detect the presence of pathogens or tissue destruction through their receptors. Cell signaling, transcription and translation follow, and these cells secrete inflammatory cytokines (e.g., tumor necrosis factor-alpha, TNF-alpha; interleukin-1,IL-1; IL-6) and chemokines (e.g., IL-8), which attract other inflammatory cells to the site. They cause fever and vasodilation, and increase capillary permeability, responsible for the clinical signs observed during inflammation (Chapter 18, Table 18.1).
The inflammatory cytokines also induce the expression of adhesion molecules called selectins (e.g., E-selectin) and integrins (e.g., vascular cell adhesion molecule-1, VCAM-1) on the luminal surface of local endothelial cells that bind (initially gently, then tightly) to the surface of leukocytes in the blood flow. This process induces the expression of similar adhesion molecules on the leukocyte surfaces (e.g., L-selectin; integrin CD11a-CD18 or LFA-1 lymphocyte-function associate antigen 1). With time, leukocytes roll along the luminal endothelium, then attach tightly to the endothelial cells and, finally, pass through gaps between them. A similar process is used in the absence of inflammation, when monocytes leave the blood stream into tissues and become resident macrophages, the immune sentinels. Once in the tissue, leukocytes follow the chemokine (e.g., interleukin-8, IL-8; complement component C5a) gradient produced by the macrophages and other inflammatory cells and proteins, and find the site of inflammation.
1.3 The immune cells and soluble molecules
The immune cells originate from myeloid and lymphoid precursors in the bone marrow, and follow stepwise genetically and epigenetically controlled lineage differentiation from hematopoietic stem cells. The bone marrow milieu has cell lineage niches that receive and respond to systemic signals (i.e., hormones, cytokines) with the production of new hematopoietic cells.
1.3.1 Myeloid cells
Myeloid cells comprise neutrophils, monocytes, macrophages, dendritic cells, eosinophils, basophils, mast cells, red cells and thrombocytes. These cells can complete maturation in the bone marrow, although further differentiation upon antigen encounter may happen at peripheral sites (e.g., monocytes differentiating into macrophages). Neutrophils, monocytes, macrophages and dendritic cells are phagocytes. They recognize pathogens, phagocytose and kill them, becoming activated during this process, and secreting cytokines and chemokines to signal other cells and expand the inflammatory response (Chapter 18, Table 18.4).
The recognition of pathogens by phagocytes is based on their pattern-recognition receptors (PRR). Signaling PRR include Toll-like receptors (TLRs, e.g., TLR-2, TLR-4, TLR-7 – about 11 described thus far); nucleotide-binding oligomerization receptors (NOD-like receptors – about 20 described thus far); or retinoic-acid inducible protein-1 (RIG-1-like receptors, also known as RLRs) (Figure 1.1; see also Chapter 18, Table 18.3). Located on the cell membrane or in the cytosol, they detect extracellular and intracellular pathogens, respectively. Each of these receptors recognizes distinct pathogen-associated molecular patterns (PAMPs), for which it has affinity.
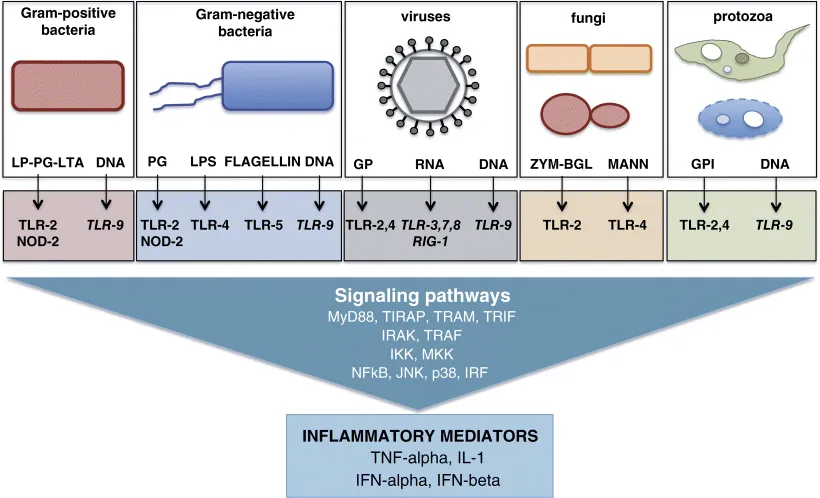
Figure 1.1 The pathogen-associated molecular patterns (PAMPs) and pathogen-pattern receptors (PRRs).
Pathogen small molecular motifs (PAMPs) or extracts (vaccines) can be detected by cell-membrane or intracellular (endosomic) receptors (PRRs) in phagocytes (e.g., macrophages and dendritic cells). PAMP-PRR binding triggers receptor-specific cell signaling events that lead to the production of inflammatory mediators (pro-inflammatory cytokines and type 1 interferons). Bacterial lipopeptide (LP), peptidoglycan (PG), lipoteichoic acid (LTA), lipopolysaccharide (LPS), and flagellin are detected by different cell-membrane toll-like receptors (TLRs) and intracellular nucleotide-binding oligomerization receptors (NOD-like receptors). Viral glycoprotein is detected by TLR-2 and TLR-4. Protozoal-released glycosylphosphatidylinositol (GPI)-anchored proteins are recognized by TLR-2 and TLR-4. Fungal zymogen and beta-glucosidase (BGL) are recognized by TLR-2, and mannose by TLR-4. Viral nucleic acids ribonucleic acid (RNA) is detected by intracellular TLR-3, TLR-7 and TLR-8, and retinoic-acid inducible protein-1 (RIG-1-like receptors); bacterial, viral and protozoal DNA (i.e., unmethylated cytosine-phosphodiester-guanine deoxynucleotide (CpG) motif) is recognized by intracellular TLR-9.
In addition, endogenous molecules released by cell damage serve as danger alert, also known as damage-associated molecular patterns (DAMPs). As signaling receptors, PRR binding to a certain PAMP induces a determined cell-signaling configuration that results in the transcription and translation of a determined type of inflammatory response. Hence, the type of pathogen, defined by its signature molecular pattern, determines the type of immune response that, hopefully, will eliminate it. Early danger signals will recruit inflammatory cells that promptly potentiate this capacity.
Phagocytosis is the process of engulfing particles (endocytosis), including organisms, cells, proteins and other molecules. Phagocytes use different receptors to initiate phagocytosis. Some of them bind directly to the pathogens (e.g., mannose-receptors), whil...
Table of contents
- Cover
- Title Page
- Copyright
- Dedication
- Contributors
- Preface
- Chapter 1: The Immune System
- Chapter 2: The Immune System of the Young Horse
- Chapter 3: The Immune System of the Older Horse
- Chapter 4: Anaphylaxis
- Chapter 5: Allergy
- Chapter 6: Immune-Mediated Cytopenias
- Chapter 7: Bullous Diseases of the Skin and Mucosa
- Chapter 8: Serum Sickness
- Chapter 9: Vasculitis
- Chapter 10: Purpura Hemorrhagica
- Chapter 11: Glomerulonephritis
- Chapter 12: Inflammatory and Immune-Mediated Muscle Disorders
- Chapter 13: Granulomatous Diseases
- Chapter 14: Chronic Inflammatory Bowel Disease
- Chapter 15: Recurrent Uveitis
- Chapter 16: Recurrent Airway Obstruction and Summer Pasture-Associated Obstructive Pulmonary Disease
- Chapter 17: Inflammatory Airway Disease
- Chapter 18: Inflammation, Endotoxemia and Systemic Inflammatory Response Syndrome
- Chapter 19: Leukemia
- Chapter 20: Lymphoma
- Chapter 21: Immunodeficiencies
- Chapter 22: Immunologic Testing
- Chapter 23: Non-Steroidal Anti-Inflammatories
- Chapter 24: Immunosuppressive Therapy
- Chapter 25: Immunomodulators
- Chapter 26: Immunoglobulin Therapy
- Chapter 27: Plasmapheresis
- Chapter 28: Principles of Vaccination
- Chapter 29: Types of Vaccines
- Chapter 30: Transplantation Immunology
- Chapter 31: Mesenchymal Stem Cell Therapy
- Chapter 32: Hematopoietic Stem Cell Transplantation
- Index
- End User License Agreement
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Equine Clinical Immunology by M. Julia B. Felippe in PDF and/or ePUB format, as well as other popular books in Medicine & Equine Veterinary Science. We have over one million books available in our catalogue for you to explore.