Acute and Critical Care Nursing at a Glance
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Acute and Critical Care Nursing at a Glance
About This Book
From the publishers of the market-leading at a Glance series comes a comprehensive yet accessible overview of all the fundamental elements of acute and critical care nursing.
Acute and Critical Care Nursing at a Glance provides an introduction to the key knowledge and skills for patient assessment and problem identification, as well as how to plan, implement and evaluate care management strategies. It also explores clinical decision-making processes and their impact on care delivery, as well as key psychosocial issues, pain management, and safe transfer. All information is presented in a clear, double-page spread with key information accompanied by tables, illustrations, photographs and diagrams.
Key features:
- Superbly illustrated, with full colour illustrations throughout
- An accessible, evidence-based, introduction to a complex topic
- Presents information structured according to the Resuscitation Council's systematic ABCDE framework for ease of understanding
- Accompanied by patient case studies to help apply theory to practice
Acute and Critical Care Nursing at a Glance is ideal for nursing students, healthcare assistants, and registered nurses working within the acute and critical care setting.
Frequently asked questions
Information
Part 1
Nursing in acute and critical care
Chapters
- 1 Critical care without walls
- 2 Recognising risk of deterioration: ABCDE assessment
- 3 Early warning tools and care escalation
- 4 Hospital-acquired infection: infection prevention and control
- 5 Pain management
- 6 Psychosocial issues
- 7 Safe transfer of the acutely unwell patient
1
Critical care without walls
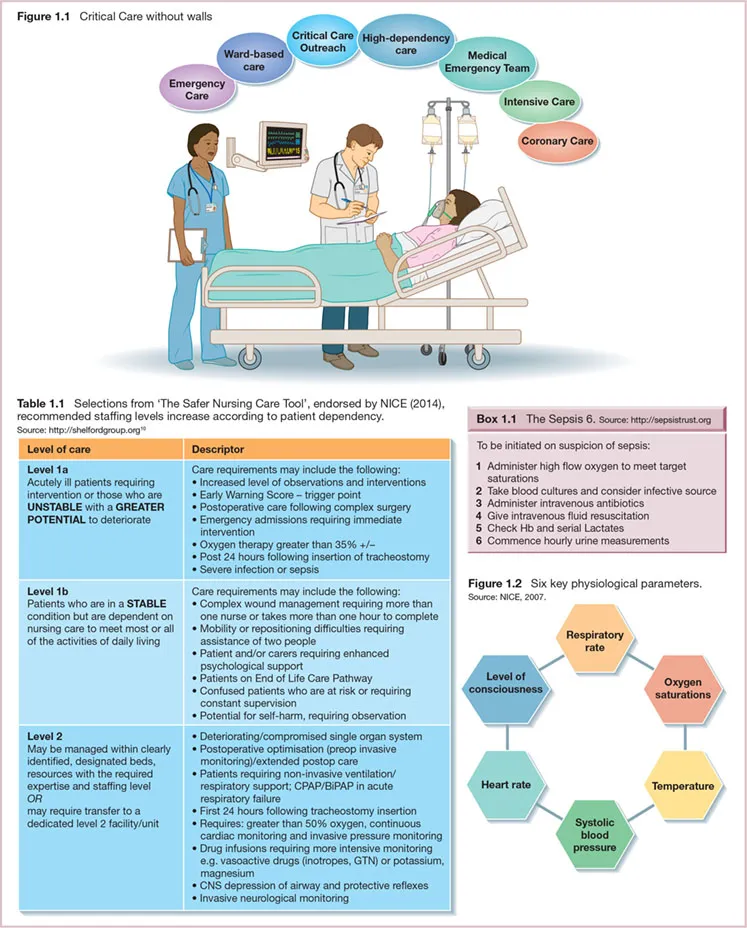
Changing patterns in acute care
Reconfiguration of critical care services
- Level 0: Patients whose needs can be met through normal care in an acute hospital.
- Level 1: Patients at risk of their condition deteriorating, or those recently relocated from higher levels of care whose needs can be met on an acute ward with advice and support.
- Level 2: Patients requiring more detailed observation or interventions, including support for single organ failure, postoperative care, and those stepping down from a higher level of care.
- Level 3: Patients requiring advanced respiratory support or support of at least two organs, including all complex patients requiring support for multiorgan failure.
Safe staffing levels
Resuscitation to medical emergency
Critical care outreach
Monitoring the acutely unwell patient
2
Recognising risk of deterioration: ABCDE assessment
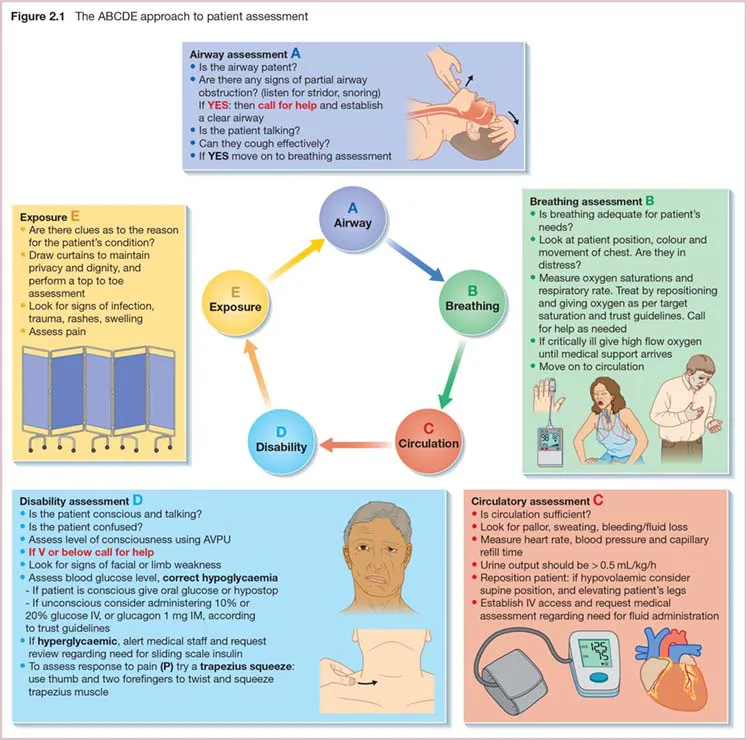
The acutely unwell patient
Table of contents
- Cover
- E-book Logo
- Title Page
- Copyright
- Contributors
- Acknowledgements
- Preface
- Abbreviations
- About the companion website
- Part 1: Nursing in acute and critical care
- Part 2: Airway: maintaining airway patency
- Part 3: Breathing: patients with breathing problems
- Part 4: Circulation: patients with circulatory problems
- Part 5: Disability: patients with neurological impairment
- Part 6: Exposure
- Part 7: Decision making in acute and critical care
- Appendix
- References and Further Reading
- Glossary
- Index
- EULA