- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Rapid Cardiac Care
About this book
Rapid Cardiac Care is an indispensable resource for all frontline staff working with acutely ill patients. Offering easy access to the knowledge base needed to provide rapid, safe and effective cardiac care, it is ideal for newly qualified healthcare professionals including, nurses, paramedics, cardiac technicians, junior medics, and physiotherapists.
Key features include:
- Essential information to support the assessment of the cardiac patient including focused history taking and physical assessment, rhythm interpretation and 12-lead ECG assessment
- Practical guidance on how to care for patients with cardiac emergencies, including acute coronary syndromes, arrhythmias, heart failure and cardiac arrest
- A quick reference A-Z section that explores a wide range of conditions affecting the heart, each with a comprehensive overview of patient presentation and strategies to guide patient assessment and management
- Diagrams and images are provided to facilitate learning
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Part 1
Cardiac Anatomy and Physiology
1
Anatomy
The heart is a cone-shaped, muscular organ with four chambers that propel blood through the circulatory system (Figure 1.1). The two upper chambers, the atria, and the ventricles below are separated by the annulus fibrosus (AV ring), a layer of connective tissue that forms the cardiac skeleton, seen on the external surface of the heart as the atrio-ventricular (AV) groove. The mitral and tricuspid (AV) valves and aortic and pulmonary (semilunar) valves form part of the AV ring. Each valve consists of two or three cusps arising from an annulus. Healthy valves maintain forward blood flow through the heart, opening and closing in response to changes in pressure between the chambers. The interatrial septum separates the two atria; the ventricles are separated by the interventricular septum, which is visible on the outside of the heart as anterior-posterior interventricular groove.
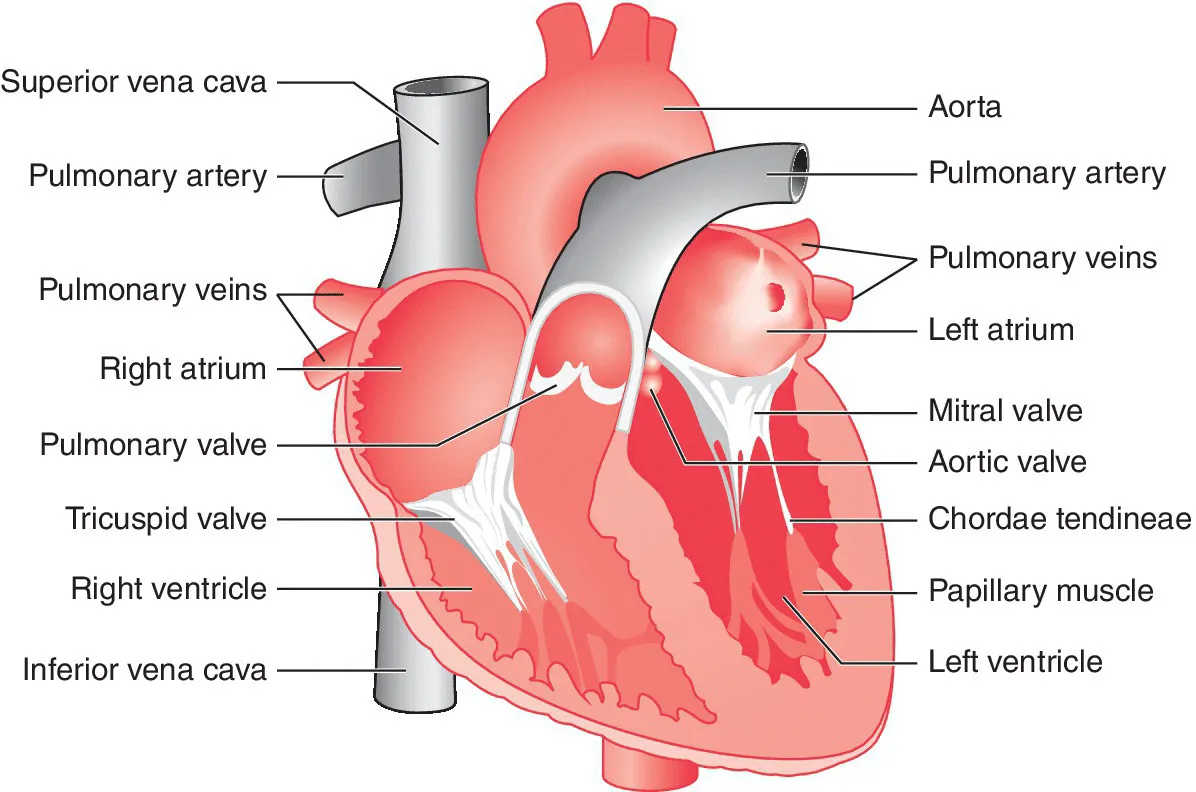
Figure 1.1 Cardiac anatomy.
The heart wall is formed from three layers of tissue that provide different functions. The external layer is the pericardium, which surrounds the heart and the roots of the aorta and pulmonary arterial trunk. It consists of two distinct layers: the outermost fibrous layer and serous layer beneath. The serous pericardium has a visceral layer, known as the epicardium, which surrounds the myocardium and doubles back on itself to form the parietal pericardium, which lines the tough, outer fibrous layer. The space between the two layers contains a small volume of fluid to reduce friction during myocardial contraction. The central, thickest layer of the heart wall is the myocardium. It contains clusters of cardiac muscle cells known as myocytes, each surrounded by connective tissue and a network of capillaries. The internal surface of the heart is lined with a single, continuous layer of endothelial cells known as the endocardium. This facilitates smooth blood flow through the chambers and across the valves and provides some protection from the formation of thrombi.
Cardiac cycle
Cardiac output is the volume of blood ejected from the left ventricle (LV) in one minute, i.e. heart rate × stroke volume. It is approximately 4–7 L/min. The cardiac conduction system controls heart rate variability and co-ordinated systolic (contraction) and diastolic (relaxation and filling) activity of the cardiac chambers to maximise cardiac output.
The superior and inferior vena cava empty into the right atrium, enabling the return of deoxygenated blood to the heart. The coronary sinus, a large cardiac vein, also drains deoxygenated blood from the myocardium into the right atrium. The tricuspid valve opens to permit blood to enter the right ventricle (RV); atrial contraction provides extra force to expel blood from the chamber, known as the ‘atrial kick’, to optimise the end diastolic volume (EDV) of the ventricles.
During systole, the three papillary muscles in the RV contract, tightening the chordae tendineae, attached to the cusps of the tricuspid valve to ensure the valve leaflets remain closed, preventing regurgitation of blood into the right atrium. Pressure within the RV will rise until it exceeds the pressure within the pulmonary circulation beyond, forcing the pulmonary valve to open and blood to flow into the pulmonary arterial trunk. During ventricular diastole, the pulmonary arteries will rapidly recoil to enable blood to fall back towards the RV, closing the pulmonary valve.
Having completed gaseous exchange within the alveoli and pulmonary capillaries, oxygenated blood returns to the left atrium via four pulmonary veins. The increase in pressure within the atrial chamber forces the mitral valve to open and ventricular filling to begin. During diastole, the ventricular myocytes will stretch to accommodate the volume of blood, which directly correlates with the force of contraction that occurs during systolic contraction (Frank Starling’s Law). The two papillary muscles contract first, once systole begins, tightening the chordae tendineae attached to the two cusps of the mitral valve to prevent regurgitation. The LV and septum then contract to increase the pressure (preload) within the LV. Once the preload pressure exceeds the pressure in the aorta beyond the aortic valve (afterload), blood will leave the LV, referred to as the stroke volume, crossing the aortic valve into the aorta to supply the arterial circulation. The term ‘ejection fraction’ refers to the stroke volume as a percentage of the left ventricular EDV (LVEDV), usually approximately 60–70% at rest. As systole ends, diastole begins again and a small volume of blood in the aorta will return towards the LV, closing the aortic valve cusps and simultaneously perfusing the coronary arteries originating at the aortic root.
Cardiac conduction system
The cardiac conduction system lies beneath the endocardium within the myocardium and consists of specialised myocytes responsible for generating and transmitting an impulse across the heart (Figure 1.2). The sino-atrial (SA) node, located on the posterior wall of the right atrium, is the primary pacemaker of the heart and therefore determines heart rate. It is capable of regular spontaneous depolarisation without external stimulus. However, the autonomic nervous system controls the SA nodal firing rate, permitting heart rate variability in response to fluctuating metabolic demand. Increased sympathetic activity will cause an increase in the SA nodal firing rate, for example during exercise. The heart rate is slowed via the vagus nerve, part of the parasympathetic nervous system.
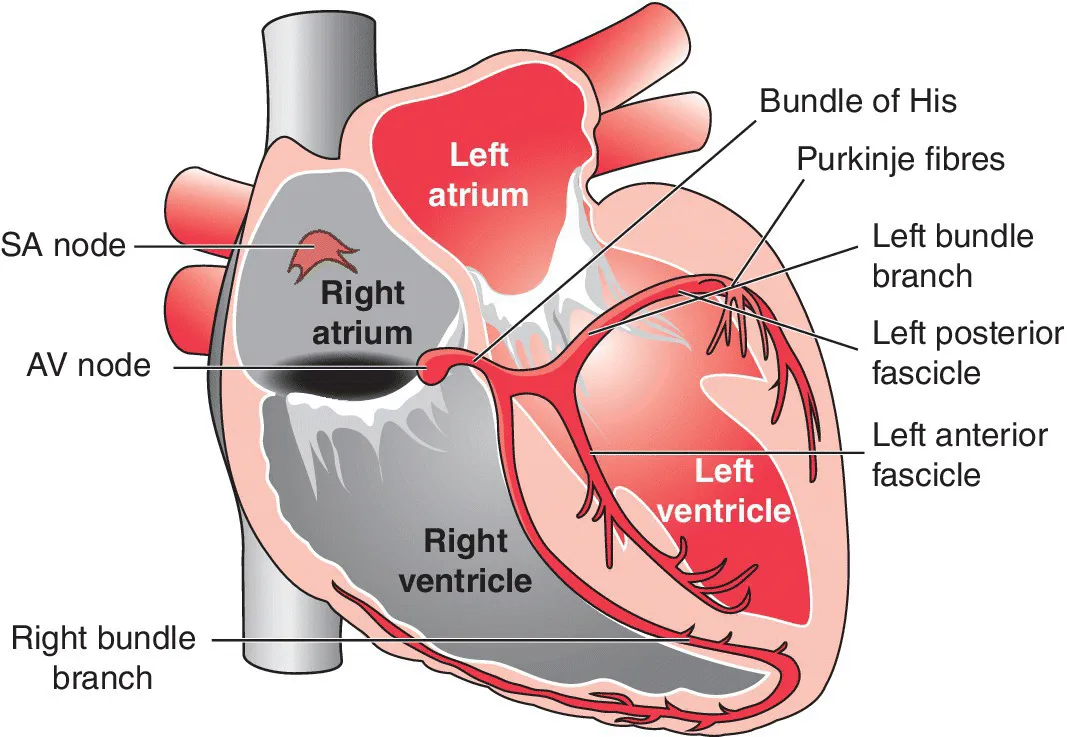
Figure 1.2 Cardiac conduction system.
Transition cells surrounding the SA node transfer the impulse across to the surrounding atrial myocytes, which in turn propagate the impulse to the remaining atrial cells, causing depolarisation and contraction. The annulus fibrosus, or AV ring, prevents direct transmission of the impulse to the ventricle. In response to atrial stimulation, the AV node transmits the impulse to the ventricular myocardium via the His-Purkinje system. After leaving the AV node, the impulse traverses the Bundle of His, which divides into two bundle branch systems. The right bundle branch is a thin, long strand, which runs down the right side of the interventricular septum and supplies conduction to the RV. The left bundle branch comprises shorter, thicker fibres, which divide into two branches called fascicles. The left anterior fascicle is the thinner of the two fascicles and supplies the septum, anterior and lateral walls of the LV. The shorter, thicker left posterior fascicle supplies the electrical impulse to the posterior wall of the LV. A network of Purkinje fibres deliver the impulse first to the papillary muscles and then rapidly across the ventricles, resulting in simultaneous contraction. If the SA node fails to fire, the AV node, His-Purkinje system and ventricular myocardium are capable of generating an electrical impulse but at a slower rate than the SA node.
Movement of ions across the cell membrane, using diffusion and active transport mechanisms, is necessary to initiate myocardial depolarisation (systole) and repolarisation (diastolic relaxation).
The movement of ions across the cell membrane, known as the cardiac action potential, is responsible for initiating myocardial depolarisation (systole) and repolarisation (relaxation). A difference in electrical charge exists across the cell membrane, created by differences in the concentration of ions in the intracellular and extracellular fluid. This is known as the transmembrane potential. During the resting phase of the cardiac cycle, the transmembrane potential is approximately –90 mV (phase 4). At this stage, there is a higher concentration of intracellular potassium and lower concentration of intracellular sodium relative to their respective extracellular levels. This creates a concentration gradient, permitting the movement of ions across the cell membrane by diffusion and altering the transmembrane potential. Once this reaches –70 mV (threshold potential), early myocardial depolarisation will be triggered. Therefore, a sodium-potassium (Na+/K+) pump within the cell membrane uses active transport to move sodium out of the cell and potassium back into the cell to maintain the resting transmembrane potential of –90 mV during phase 4.
Myocardial depolarisation begins when sodium channels within the cell membrane open, permitting entry of sodium into the cell (phase 0). Once the transmembrane potential reaches the threshold potential of approximately –70 mV, fast sodium channels open, increasing the transmembrane potential to +30 mV. Repolarisation of the cell begins immediately afterwards, with a slight drop in transmembrane potential due to the closure of the sodium channels and an influx of chloride ions (phase 1). Myocardial contraction is maintained through the influx of calcium ions into the cell, causing the transmembrane potential to plateau at approximately 0 mV (phase 2). Repolarisation continues as the potassium channels open, allowing potassium to leave the cell, causing a dramatic fall in transmembrane potential (phase 3) until the resting membrane potential of –90 mV is reached and maintained using the Na+/K+ pump, rendering the cell inactive again (phase 4).
Coronary circulation
Situated within the epicardium, the coronary arterial circulation is a network of arteries, arterioles and capillaries that penetrate the...
Table of contents
- Cover
- Title Page
- Table of Contents
- List of Abbreviations
- Preface
- Acknowledgements
- Part 1: Cardiac Anatomy and Physiology
- Part 2: Rapid Cardiac Assessment
- Part 3: Rapid 12-lead ECG Interpretation
- Part 4: Cardiac Conditions A–Z
- Index
- End User License Agreement
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Rapid Cardiac Care by Emma Menzies-Gow,Christine Spiers in PDF and/or ePUB format, as well as other popular books in Medicine & Nursing. We have over one million books available in our catalogue for you to explore.