Integrated Care
Creating Effective Mental and Primary Health Care Teams
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Integrated Care
Creating Effective Mental and Primary Health Care Teams
About This Book
An integrated, collaborative model for more comprehensive patient care
Creating Effective Mental and Primary Health Care Teams provides the practical information, skills, and clinical approaches needed to implement an integrated collaborative care program and support the members of the care team as they learn this new, evidence-based, legislatively mandated care delivery system. Unique in presenting information specifically designed to be used in an integrated, collaborative care workflow, this book provides specific guidance for each member of the team. Care managers, consulting psychiatrists, primary care providers, and administrators alike can finally get on the same page in regard to patient care by referring to the same resource and employing a common framework. Written by recognized experts with broad research, clinical, implementation, and training experience, this book provides a complete solution to the problem of fragmented care.
Escalating costs and federal legislation expanding access to healthcare are forcing the industry to transition to a new model of health care delivery. This book provides guidance on navigating the changes as a team to provide the best possible patient care.
- Integrate physical and behavioral care
- Use evidence-based treatments for both
- Exploit leading-edge technology for patient management
- Support each member of the collaborative care team
Strong evidence has demonstrated the efficacy of a collaborative care approach for delivering mental health care to patients in a primary care setting. The field is rapidly growing, but few resources are available and working models are limited. This book provides a roadmap for transitioning from traditional methods of health care to the new integrated model. Providers ready to move to the next level of care will find Creating Effective Mental and Primary Health Care Teams an invaluable resource.
Frequently asked questions
Information
Chapter 1
Working as a Team to Provide Collaborative Care
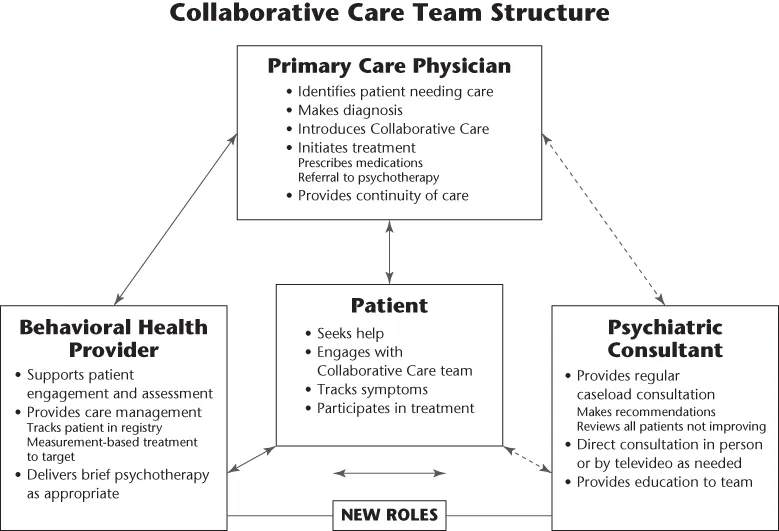
Collaborative Care team roles
- Patient
- The most important person on the team!
- Works with the primary care provider (PCP) and the behavioral health provider (BHP)/care manager (CM).
- Reports changes in health, symptoms, and functioning.
- Sets goals for treatment with the team.
- Tracks clinical progress using patient-reported outcome measures.
- Asks questions and discusses concerns about care.
- Understands treatment plan, including goals of behavioral interventions and names/doses of medications.
- Primary care provider (PCP)
- Clinician degrees may include MD, DO (doctor of osteopathic medicine), ARNP (advanced registered nurse practitioner), and NP (nurse practitioner).
- Oversees all aspects of patient's care.
- Introduces Collaborative Care team, often with “warm handoff.”
- Diagnoses common mental disorders.
- Prescribes medications to treat psychiatric illnesses as appropriate.
- Adjusts treatment in consultation with BHP/care manager, psychiatric consultant, and other behavioral health providers.
- Behavioral health provider (BHP)
- Clinician degrees may include MSW, LCSW, RN, MA, PhD, and PsyD.
- Works closely with PCP and helps manage a caseload of patients in primary care (care manager).
- Facilitates patient engagement and education.
- Performs structured initial and follow-up assessments.
- Systematically tracks treatment response using behavioral health measures.
- Provides brief, evidence-based behavioral interventions or refers to other BHP for these services.
- Supports medication management by PCPs.
- Helps patient identify where to get medications.
- Encourages and supports medication adherence.
- Brings concerns about medications or side effects to PCP, and schedules PCP visit to adjust treatments as appropriate.
- Reviews challenging patients in systematic, weekly case review with the psychiatric consultant.
- Facilitates referrals to other services (e.g., substance abuse treatment, specialty care, and community resources) as needed.
- Prepares patient for relapse prevention.
- Psychiatric consultant (PC)
- Psychiatrist or other expert in psychiatry and psychopharmacology.
- Supports PCPs and BHPs, providing regular (weekly) and as-needed consultation on a caseload of patients followed in primary care.
- Focuses on patients who are not improving and who need treatment adjustment or intensification.
- Available to provide in-person or telemedical consultation or, for complex or persistently ill patients, referral.
- Provides education and training for primary care providers and BHPs as appropriate.
- Other behavioral health providers
- These may include chemical dependency counselors or other licensed behavioral health professionals.
- Deliver specialized evidence-based counseling/psychotherapy (individual or group).
- Support behavioral health interventions focused on health behaviors.
- Provide chemical dependency counseling/treatment.
- Facilitate other mental health or substance abuse services.
- Other partners important to include in team building
- CEO, administrators, medical directors, clinic managers.
- Medical and mental health leaders/champions.
- Receptionists/front desk staff, medical assistants.
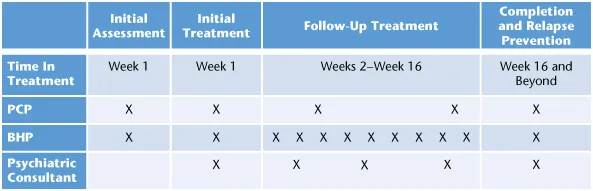
Collaborative Care shared workflow
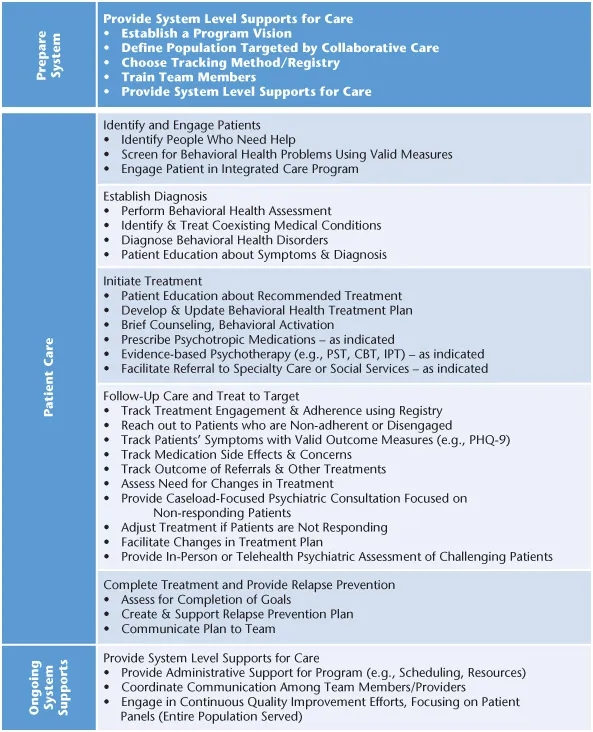
Core Collaborative Care skills and tools
Introducing the Collaborative Care team approach to the patient
- The patient is an important member of the team.
- All team members will share one treatment plan to support patie...
Table of contents
- Cover
- Title Page
- Copyright
- Table of Contents
- Dedication
- Preface Using Collaborative Care to Create Effective Mental and Primary Health Care Teams
- Acknowledgments
- Chapter 1: Working as a Team to Provide Collaborative Care
- Part 1: Collaborative Care for Common Primary Care Presentations
- Part 2: Collaborative Care Interventions
- Appendix: Resources
- About the Authors and Contributors
- Index
- End User License Agreement