eBook - ePub
A Practical Manual of Diabetic Retinopathy Management
This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
A Practical Manual of Diabetic Retinopathy Management
Book details
Book preview
Table of contents
Citations
About This Book
The incidence of diabetes is increasing worldwide at an alarming rate, and diabetic retinopathy is one of the most significant complications of diabetes. Packed with outstanding retinal photos, the second edition of this one-stop clinical manual offers a comprehensive overview of the diagnosis, treatment and long–term management of patients with diabetic eye disease.
Edited and authored by world-renowned experts from leading centres of excellence, A Practical Manual of Diabetic Retinopathy Management presents evidence-based guidance relevant for a global audience of health-care professionals, including diabetologists, ophthalmologists, retinal screeners, optometrists, ophthalmic nurses, GPs, and medical students.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access A Practical Manual of Diabetic Retinopathy Management by Peter H. Scanlon, Ahmed Sallam, Peter van Wijngaarden, Peter H. Scanlon, Ahmed Sallam, Peter van Wijngaarden in PDF and/or ePUB format, as well as other popular books in Medicine & Endocrinology & Metabolism. We have over one million books available in our catalogue for you to explore.
Information
Chapter 1
Introduction
Peter H. Scanlon
Harris Manchester College, University of Oxford; Medical Ophthalmology, University of Gloucestershire, UK
In this book the fundamental approach is to describe the classification of diabetes, risk factors for diabetic retinopathy and lesions of diabetic retinopathy, and explain the significance of these lesions in terms of progression of the disease, recommended treatment and consequences to vision. Methods of screening for diabetic retinopathy and other retinal conditions that are more frequent in diabetes, or have similar appearances to diabetic retinopathy, are also discussed.
The four main themes in this introductory chapter are: (1) practical assessment consisting of history and examination; (2) multidisciplinary management; (3) investigative techniques to assess diabetic retinopathy; and (4) the use of lasers in diabetic retinopathy.
PRACTICAL ASSESSMENT
History
The history of the patient can be divided into the following sections: presenting complaint; past ocular history; diabetic history; past medical history; family history; drug history; and psychosocial history.
Presenting complaint
Many patients with diabetic retinopathy are asymptomatic until the more advanced stages of the disease. When symptoms do occur they are usually a gradual blurring of vision in diabetic maculopathy and a sudden onset of visual symptoms with a vitreous haemorrhage. Patients notice a streak or a sudden onset of floaters in one eye, which increases with progressive visual loss over the next hour as the vitreous haemorrhage progresses. The amount of visual loss depends on the amount or position of the vitreous haemorrhage. If the vitreous or preretinal haemorrhage is in the visual axis of the eye, then visual loss is usually quite marked.
Past ocular history
The past ocular history of patients covers: (1) visual symptoms; (2) cataract or strabismus surgery; (3) laser treatment; and (4) vitrectomy.
Diabetic history
The diabetic history of a patient includes: (1) type of diabetes; (2) duration of diabetes; and (3) treatment of diabetes (e.g. diet, oral hypoglycaemics, insulin or a combination).
Complications of diabetes
The complications of diabetes can fall within three categories: (1) nephropathy (renal impairment, peritoneal dialysis, haemodialysis); (2) cardiovascular (angina, myocardial infarction, coronary artery bypass); and (3) cerebrovascular (transient ischaemic attack, stroke).
Past medical history
Past medical history can include serious illnesses and operations.
Drug history
Patients should disclose drug history such as present medication and any allergies.
Family history
Any history of diabetes or other illnesses in the family should be discussed.
Psychosocial
The patient's physosocial factors, such as occupation, number of cigarettes smoked per day, units of alcohol consumed per day, history of psychiatric illness and home circumstances (e.g. type of accommodation, whether lives alone, etc.), must be considered.
Eye examination
Assessment of visual acuity
The first part of the eye examination is an assessment of visual acuity (VA). A Snellen or LogMar chart is used and should be back surface illuminated in order to provide accurate measurements (see Figs 1.1 and 1.2).
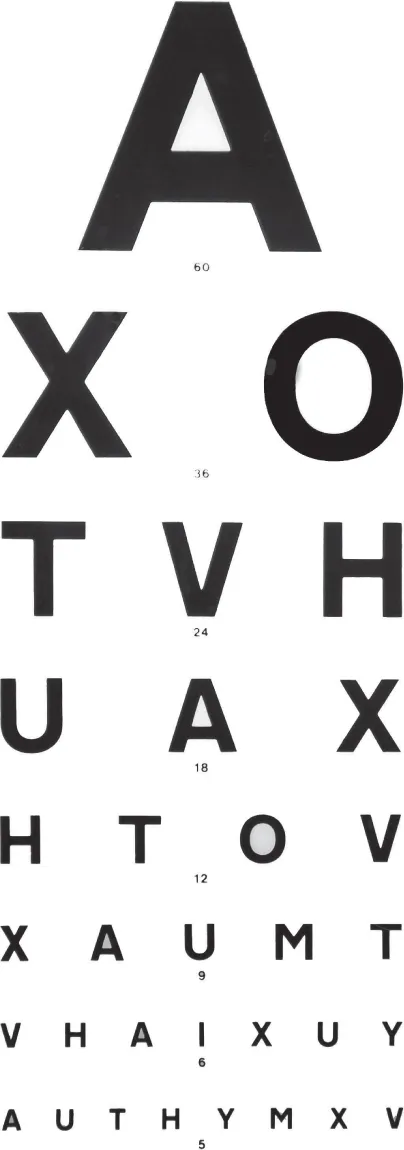
Fig. 1.1 Snellen visual acuity chart.
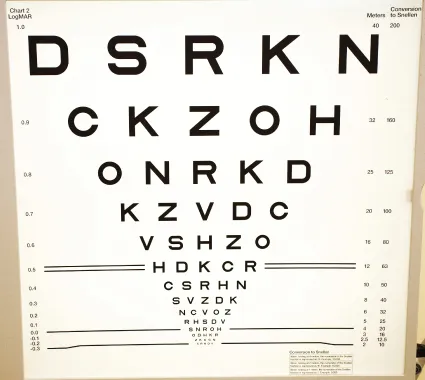
Fig. 1.2 LogMar visual acuity chart.
The unaided VA is recorded first. The VA with current distance spectacle correction is then recorded. Finally, the VA with current distance spectacle correction and a pinhole is recorded. The best of these three measurements is recorded as the best corrected visual acuity. A refraction may be performed if required.
Assessment of colour vision
People with diabetes can develop an acquired colour vision defect (typically a blue loss initially) prior to showing any significant features of diabetic retinopathy. I have seen one patient who appeared to have mild non-proliferative diabetic retinopathy who had developed pronounced loss of colour vision; this meant that he was unable to continue in his current employment as a train driver.
The most appropriate test for identifying and quantifying acquired colour vision loss is the Farnsworth-Munsell 100 hue discrimination test (see Fig. 1.3). In clinical practice, however, this test is often not available and the Ishihara test, which is designed for detecting congenital (red/green) colour vision defects, is applied. If the Ishihara test is used for the assessment of acquired colour vision defects, clinicians need to be cautious when interpreting test results since it produces a high false-negative rate; passing the test is not necessarily consistent with normal colour vision.
Inspection of external structures
An inspection of external structures includes comparing one eye with the other to detect unilateral abnormalities and to determine whether the opening between the lids is symmetrical. The margins of the eyelids are inspected for ingrowing eye lashes, inversion or eversion, mucus, discharge, scales or lumps. The conjunctival lining is inspected in each eye and the area over the lacrimal sac at the medial corner of the lower lids and nose on each side.
Visual fields to confrontation
The patient must cover one eye and stare at the examiner's eye. The examiner's finger/hand or an object such as a hat pin with a white or coloured head will then be moved out of the patient's visual field and be brought back in, and the patient asked to indicate when the finger/hand or object comes back into view. This can be used as a simple preliminary test and can be useful particularly if a hemianopia is suspected. More minor deg...
Table of contents
- Cover
- Title Page
- Copyright
- Table of Contents
- List of contributors
- Prologue
- Acknowledgements
- About the companion website
- Chapter 1: Introduction
- Chapter 2: Diabetes
- Chapter 3: Lesions and classifications of diabetic retinopathy
- Chapter 4: Screening for diabetic retinopathy
- Chapter 5: Imaging techniques in diabetic retinopathy
- Chapter 6: The normal eye
- Chapter 7: Diabetic macular oedema
- Chapter 8: Mild non-proliferative diabetic retinopathy
- Chapter 9: Moderate and severe non-proliferative diabetic retinopathy
- Chapter 10: Proliferative and advanced diabetic retinopathy
- Chapter 11: Proliferative diabetic retinopathy with maculopathy
- Chapter 12: The stable treated eye
- Chapter 13: Vitrectomy surgery in diabetic retinopathy
- Chapter 14: Cataract surgery in the diabetic eye: Pre-, intra- and postoperative considerations
- Chapter 15: Pregnancy and the diabetic eye
- Chapter 16: Low vision and blindness from diabetic retinopathy
- Chapter 17: Future advances in the management of diabetic retinopathy
- Chapter 18: Other retinal conditions in diabetes
- Chapter 19: Conditions with appearances similar to diabetic retinopathy
- Glossary
- Index
- End User License Agreement