- English
- ePUB (mobile friendly)
- Available on iOS & Android
Midwifery at a Glance
About this book
Midwifery at a Glance offers an easy-to-read yet comprehensive overview of everything a midwifery student needs to know, from conception to care of the newborn.
This practical guide provides coverage of normal pregnancy, maternal and foetal physiology, and pre-existing medical conditions and how these affect pregnancy and birth. It also features vital information on the role of the midwife, evidence-based practice, health promotion education, and perinatal mental health, as well as neonatal care and an overview of emergency situations.
Midwifery at a Glance:
- Contains superb full colour illustrations throughout
- Is written specifically for midwifery students and includes all the concepts found on the midwifery curriculum
- Demonstrates links with other relevant multidisciplinary healthcare professionals
Midwifery at a Glance is the ideal guide, offering educational support for midwifery students in the application of midwifery knowledge into clinical practice.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Part 1
Introduction
- 1 Historical overview of midwifery
- 2 NHS values
- 3 Ethics
- 4 Role of the midwife
- 5 Drug exemptions
- 6 Women’s choice and care options
1
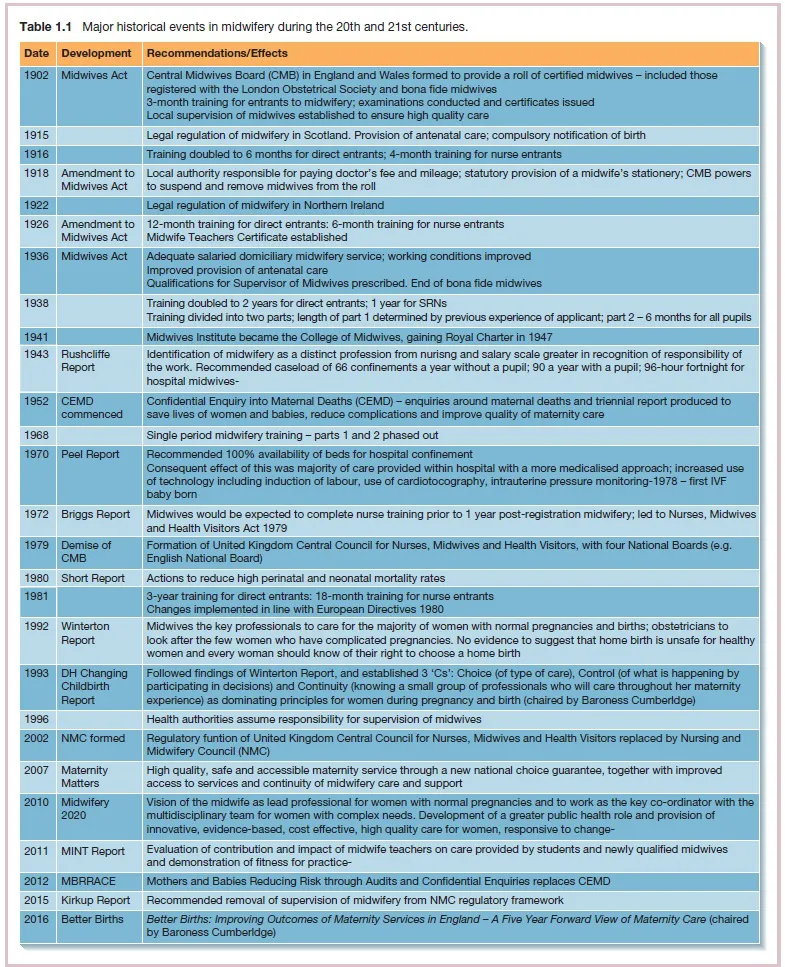
Historical overview of midwifery
2
NHS values
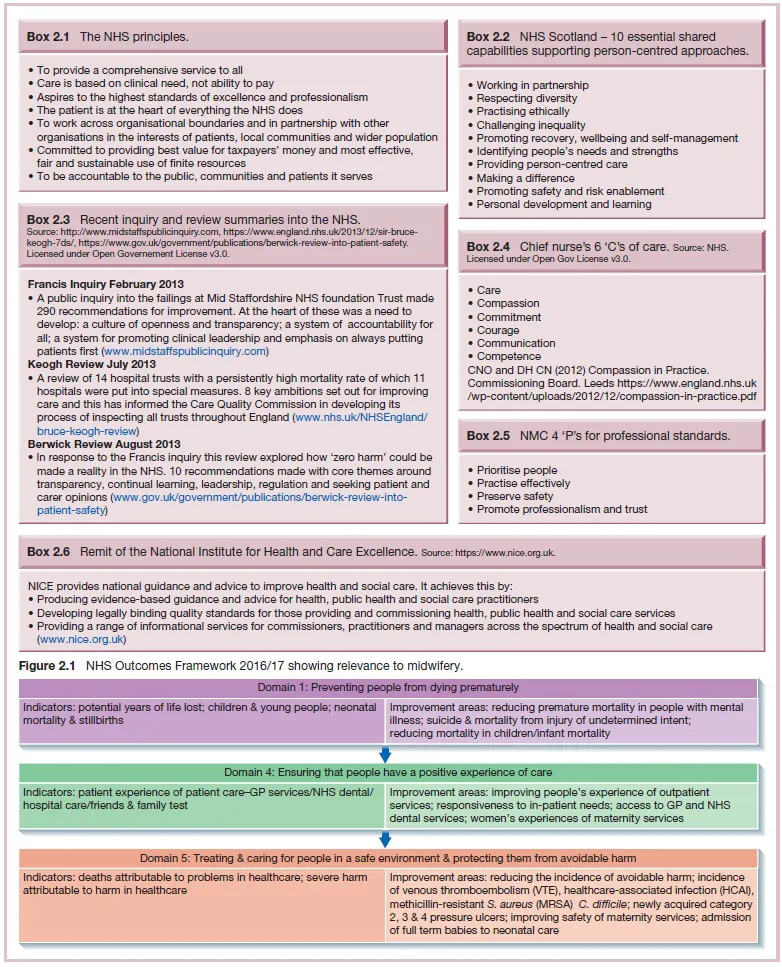
Six values
- Respect and dignity – every person is valued as an individual and respect is given to their aspirations and commitments in life, and their priorities, needs, abilities and limits should be understood, irrespective of whether they are a mother/baby, family member or staff. Care should be provided with honesty and integrity and listening to the views of others, for example when formulating a birth plan, to enhance provision of safe and effective care.
- Compassion – midwives should respond with humanity and kindness to each mother's need, pain or distress and find things that will provide comfort and relieve suffering to mothers and their families but also their colleagues, for example during labour and in times of bereavement.
- Working together for patients – mothers, babies and their family come first in everything a midwife does. Collaboration with the multidisciplinary team and networking plus seeking the views of service users will contribute to effective care delivery.
- Improving lives – the public health role of the midwife and health promotion can affect the mother's health. Midwives can innovate and improve care to improve health and wellbeing plus the mother's experience of the NHS, for example establishing teams to support vulnerable women.
- Everyone counts – midwives should maximise resources for the benefit of the whole community of mothers, babies and their families, whatever their social or educational background, their race, religion or culture; for example all women should have equal access to antenatal classes.
- Commitment to quality of care – midwives must provide safe and effective care. The right care, in the right way at the right time is dependent upon midwives' knowledge and skills, com...
Table of contents
- Cover
- Title Page
- Copyright
- Contributors
- About the companion website
- Part 1 Introduction
- Part 2 Anatomy and physiology
- Part 3 Preconception
- Part 4 Antenatal
- Part 5 Intrapartum
- Part 6 Postnatal care
- Part 7 Common medical disorders
- Part 8 Obstetric complications
- Part 9 Fetus and baby
- Part 10 Psychological dimensions
- Part 11 Midwifery skills
- References and further reading
- Index
- End User License Agreement
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app