Hypoglycaemia in Clinical Diabetes
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Hypoglycaemia in Clinical Diabetes
About This Book
Hypoglycaemia in Clinical Diabetes
Hypoglycaemia in Clinical Diabetes
Third Edition
If you regularly see patients with diabetes who experience hypoglycaemia and need expert guidance, then this is the book for you.
Hypoglycaemia in Clinical Diabetes, Third Edition once again provides health professionals involved in the management of people with diabetes with an expertly written, comprehensive guide to hypoglycaemia, the most common and feared side effect of insulin treatment for diabetes.
With reference to ADA and EASD guidelines throughout, topics covered include the physiology of hypoglycaemia and the body's response to low blood glucose, its presentation and clinical features, potential morbidity and optimal clinical management in order to achieve and maintain good glycaemic control.
Particular attention is paid to the way hypoglycaemia is managed in different groups of patients, such as the elderly, in children, or during pregnancy.
New chapters in this edition include:
- Psychological effects of hypoglycaemia
- Technology for hypoglycaemia: CSII and CGM
- Exercise management and hypoglycaemia in type 1 diabetes
- Neurological sequelae of hypoglycaemia
Valuable for diabetologists, endocrinologists, non-specialist physicians and general practitioners, Hypoglycaemia in Clinical Diabetes, Third Edition provides expert clinical guidance to this extremely common and potentially serious complication associated with diabetic management.
Titles of related interst
Diabetes: Chronic Complications, 3rd edition Shaw, ISBN 9780470656181
Diabetes Emergencies: Diagnosis and Clinical Management Katsilambros, ISBN 9780470655917
Frequently asked questions
Information
Normal Glucose Homeostasis
- Glycogen synthesis and breakdown (glycogenolysis): Glycogen, a carbohydrate, is the most readily accessible energy store and is mostly found in liver and skeletal muscle. Liver glycogen is broken down to provide glucose for all tissues, whereas the breakdown of muscle glycogen results in lactate formation.
- Gluconeogenesis: This is the production of glucose in the liver from precursors: glycerol, lactate and amino acids (in particular alanine). The process can also occur in the kidneys, but this site is not important under most physiological conditions.
- Glucose uptake and metabolism (glycolysis) by skeletal muscle and adipose tissue.
| Liver | |
| ↑ | glycogen synthesis (↑ glycogen synthetase activity) |
| ↑ | glycolysis |
| ↑ | lipid formation |
| ↑ | protein formation |
| ↓ | glycogenolysis (↓ phosphorylase activity) |
| ↓ | gluconeogenesis |
| ↓ | ketone formation |
| Muscle | |
| ↑ | uptake of glucose |
| ↑ | uptake of amino acids |
| ↑ | uptake of ketone |
| ↑ | uptake of potassium |
| ↑ | glycolysis |
| ↑ | synthesis of glycogen |
| ↑ | synthesis of protein |
| ↓ | protein catabolism |
| ↓ | release of amino acids |
| Adipose tissue | |
| ↑ | uptake of glucose |
| ↑ | uptake of potassium |
| ↑ | storage of triglyceride |
| Liver | |
| ↑ | glycogenolysis |
| ↑ | gluconeogenesis |
| ↑ | extraction of alanine |
| ↑ | ketogenesis |
| No significant peripheral action | |
Fasting (Figure 1.1a)
- Muscle: Glucose uptake and oxidative metabolism are reduced and fatty acid oxidation increased. Amino acids are released.
- Adipose tissue: There are reductions in glucose uptake and triglyceride storage. The increase in the activity of the enzyme hormone-sensitive lipase, results in hydrolysis of triglyceride to glycerol (a gluconeogenic precursor) and fatty acids, which can be metabolised.
- Liver: Increased cAMP concentrations result in increased glycogenolysis and gluconeogenesis thus increasing hepatic glucose output. The uptake of gluconeogenic precursors (i.e. amino acids, glycerol, lactate and pyruvate) is also increased. Ketone bodies are produced in the liver from fatty acids. This process is normally inhibited by insulin and stimulated by glucagon, thus the hormonal changes during fasting lead to an increase in ketone production. Fatty acids are also a metabolic fuel used by the liver as a source of energy needed for the reactions involved in gluconeogenesis.
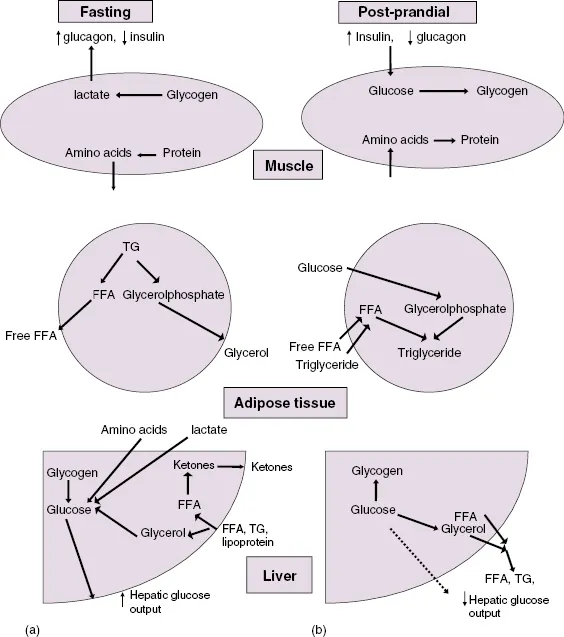
Fed state (Figure 1.1b)
- Muscle: Insulin increases glucose transport, oxidative metabolism and glycogen synthesis. Amino acid release is inhibited and protein synthesis increased.
- Adipose tissue: In the fat cells, glucose transport is increased, while lipolysis is inhibited. At the same time the enzyme lipoprotein lipase, located in the capillaries, is activated and causes triglyceride to be broken down to fatty acids and glycerol. The fatty acids are taken up into the fat cells and re-esterified to triglyceride (using glycerol phosphate derived from glucose) before being stored.
- Liver: Glucose uptake is increased in proportion to plasma glucose, a process that does not need insulin. However, insulin does decrease cAMP concentrations, which result in an increase in glycogen synthesis and the inhibition of glycogenolysis and gluconeogenesis. These effects ‘retain’ excess glucose as glycogen in the liver.
Table of contents
- Cover
- Title page
- Copyright page
- List of Contributors
- Preface
- 1: Normal Glucose Metabolism and Responses to Hypoglycaemia
- 2: Symptoms of Hypoglycaemia and Effects on Mental Performance and Emotions
- 3: Counterregulatory Deficiencies in Diabetes
- 4: Frequency, Causes and Risk Factors for Hypoglycaemia in Type 1 Diabetes
- 5: Nocturnal Hypoglycaemia
- 6: Impaired Awareness of Hypoglycaemia
- 7: Risks of Intensive Therapy
- 8: Management of Acute and Recurrent Hypoglycaemia
- 9: Technology for Hypoglycaemia: CSII and CGM
- 10: Hypoglycaemia in Children with Diabetes
- 11: Hypoglycaemia During Pregnancy in Women with Pregestational Diabetes
- 12: Hypoglycaemia in Type 2 Diabetes and in Elderly People
- 13: Mortality, Cardiovascular Morbidity and Possible Effects of Hypoglycaemia on Diabetic Complications
- 14: Long-Term Effects of Hypoglycaemia on Cognitive Function in Diabetes
- 15: Neurological Sequelae of Hypoglycaemia
- 16: Psychological Effects of Hypoglycaemia
- 17: Exercise Management and Hypoglycaemia in Type 1 Diabetes
- 18: Living with Hypoglycaemia
- Index