The perineum
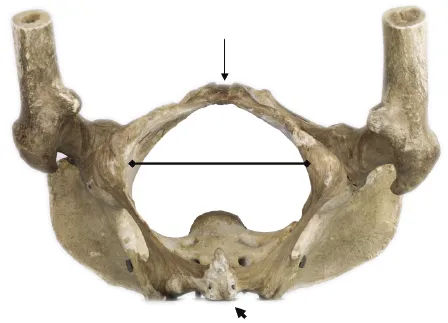
The male external genital organs comprise the penis, scrotum and scrotal contents. Any detailed description of the anatomy of the external genitalia, whether in the male or in the female, would be incomplete without a preliminary consideration of the anatomy of the perineum. The perineum refers to the lowest part of the trunk. It lies immediately below the pelvic floor (levator ani) and is flanked by the inner aspect of the proximal ends of the thighs and also by the inferior parts of the buttocks. When the thighs and buttocks are parted, the perineum may be pictured as lying within the osseo-ligamentous framework of the inferior pelvic aperture. This framework has a diamond-shaped outline (Figure 1.1): the four angles of the diamond being the sub-pubic angle anteriorly (long arrow), the coccyx posteriorly (short arrow) and the right and left ischial tuberosities on either side. The four sides of the diamond are the right and left ischiopubic rami anterolaterally, and the inferior edges of the right and left sacro-tuberous ligaments posterolaterally (Figure 1.1).
A transverse line drawn between the anterior ends of the right and left ischial tuberosities is seen to divide the perineum into two triangular divisions. The anterior division is the smaller of the two and is known as the urogenital triangle (urogenital region) of the perineum, while the larger posterior division is the anal triangle (anal region) of the perineum. The anal triangle of the perineum is similar in the two sexes, and contains the centrally located anal canal flanked by the right and left ischioanal (ischiorectal) fossae.
Stretching across the width of the urogenital triangle of the perineum from the inner surface of one ischiopubic ramus to the other is a distinct fascial layer termed the perineal membrane. The perineal membrane is quadrangular in outline and is confined to the urogenital triangle of the perineum (Figure 1.2).
It serves to demarcate the two principal subdivisions of the urogenital triangle: the deep perineal pouch and superficial perineal pouch. The former lies deep to (i.e. above) the perineal membrane and contains the membranous urethra, external urethral sphincter (the voluntary, striated muscle sphincter) and the deep transverse perinei muscles. Additionally, in the male, the bulbo-urethral glands (Cowper's glands) are situated in the deep perineal pouch, posterolateral to the membranous urethra. The ducts of the bulbo-urethral glands, however, penetrate the perineal membrane and open into the bulbous urethra in the superficial perineal pouch.
The superficial perineal pouch lies superficial to (i.e. below) the perineal membrane. This demarcation into the superficial and deep perineal pouches is more apparent in the male subject (owing to the perineal membrane being a more readily demonstrable entity in the male). The male external genitalia are situated entirely in the superficial perineal pouch. The gap between the anterior edge of the perineal membrane and the inferior border of the pubic symphysis transmits the deep dorsal vein of penis (or the dorsal vein of clitoris in the female).
Terminology in relation to the fascial layers in the urogenital region of the perineum
The membranous layer of superficial fascia in the anterior abdominal wall (Scarpa's fascia) is continued into the urogenital triangle of the perineum in both sexes as the superficial perineal fascia. In the male, this superficial perineal fascial layer is prolonged into the scrotum as the dartos fascia (tunica dartos) and contains smooth muscle on its surface. The prolongation of the superficial perineal fascia over the penile shaft is termed the superficial penile fascia, while the remainder of the superficial perineal fascia is attached to the posterior edge of the perineal membrane and to the outer margins of the everted ischiopubic rami and is termed Colles' fascia. The superficial perineal pouch is the space between the perineal membrane and the overlying superficial perineal fascia. In the male it contains the root of the penis and the associated muscles. As the superficial perineal fascia is continued into the scrotum and around the penile shaft, the superficial perineal pouch may be said to include also the scrotal contents and the penile shaft.
Deep to the superficial penile fascia is a distinct fascial layer which encircles the erectile columns (i.e. the fused corpora cavernosa and corpus spongiosum) in the penile shaft. This is the deep fascia of the penis, known also as Buck's fascia. Traced proximally, Buck's fascia is seen to be continuous with the deep fascia that covers the muscles that overlie the root of the penis, termed Gallaudet's fascia.
The principal blood supply to the perineum is derived from the right and left deep internal pudendal arteries, each being a terminal branch of the corresponding internal iliac artery's anterior division. Venous drainage is to the ipsilateral internal pudendal vein which in turn drains to the internal iliac vein. The motor innervation of all the voluntary muscles in the perineum as well as the cutaneous innervation of much of the perineum is a function of the right and left pudendal nerves. The pudendal nerve is a branch of the sacral plexus and has a root value of S2, S3 and S4.
The internal pudendal artery and pudendal nerve may therefore be spoken of as the artery and nerve of the perineum, respectively. Both these structures originate in the pelvic cavity (i.e. above the pelvic floor). They leave the pelvic cavity through the ipsilateral greater sciatic foramen (a large opening in the posterolateral aspect of the pelvic wall). Turning sharply around the tip of the ischial spine, the nerve, artery (and companion vein) run forwards below the pelvic floor to enter a fascial sleeve (the pudendal canal) within the obturator fascia in the lateral wall of the perineum.
The scrotum and scrotal contents
The scrotum is a pendulous, cutaneous sac that contains the testes, epididymes and the lower ends of the spermatic cords with their associated coverings. The scrotum is, in effect, an extension of skin and subcutaneous tissue of the anterior abdominal wall into the urogenital part of the perineum. It is suspended below the pubic arch and lies postero-inferior to the root of the penis.
The skin of the scrotum is hair-bearing and relatively thin and is generally more pigmented than the adjacent skin of the thigh and pubic region. It contains numerous sweat glands and sebaceous glands. The scrotum is devoid of subcutaneous fat; a feature that is thought to play a significant part in maintaining the intrascrotal temperature somewhat below the core temperature which is required for normal spermatogenesis. The rugosity of the scrotal skin is due to the contraction of the underlying dartos muscle.
A median septum within the scrotum divides the scrotum into right and left compartments. The septum is essentially an infolding of the dartos layer of the scrotum. The left hemiscrotum typically hangs somewhat lower than the right. The position of the intrascrotal septum is indicated on the surface by a narrow, midline ridge termed the median scrotal raphe. This raphe is continuous anteriorly with the penile raphe (on the undersurface of the penis), and posteriorly with the perineal raphe (which extends backwards almost to the anterior margin of the anal verge). Immediately deep to the dartos fascia and within each hemiscrotum are the three fascial coverings of the spermatic cord, concentrically arranged and closely applied to each other. From outside in they are the external spermatic fascia, cremasteric fascia and internal spermatic fascia. Within the latter is the tunica vaginalis testis, a thin-walled, double-layered serous membrane containing a film of fluid between the two layers. The tunica is applied to the front and sides of the testis and epididymis.
The testis is an ovoid, firm organ with its long axis vertically orientated. It is enveloped in a thick, pale fibrous covering termed the tunica albuginea. The tunica sends multiple septa into the testicular substance, breaking up the latter into numerous lobules each containing two to three highly convoluted seminiferous tubules. The seminiferous tubules from the various lobules converge posteriorly upon the rete testis, a plexiform structure. From the rete testis 12–15 ducts (vasa efferentia) penetrate the tunica albuginea and empty into the head of the epididymis. The epididymis is a firm structure but softer to the feel than the testis. It serves as a receptacle for the storage and maturation of spermatozoa. The epididymis is applied to the posterolateral aspect of the testis, and appreciation of this topographic relationship is of importance in the clinical diagnosis of testicular and epididymal conditions. The testis is supplied by the testicular artery, a direct branch of the abdominal aorta. Running down the posterior abdominal wall, the testicular artery enters the inguinal canal through the deep inguinal ring and emerges at the superficial inguinal ring to enter the spermatic cord along with the other contents of the spermatic cord (testicular lymphatics, vas deferens, artery to the vas, pampiniform plexus/testicular veins, sympathetic nerve fibers, cremasteric artery, genital branch of the genitofemoral nerve).
The large, upper end of the epididymis is the head (or globus major) and the narrow, lower pole is the tail (or globus minor). The intervening part is termed the body of the epididymis. Apart from the vasa efferentia, which run from the rete testis to the head of the epididymis, there is no direct physical connection between the testis and epididymis. The narrow slit-like space between the two is termed the sinus of the epididymis. The blood supply of the epididymis is from the testicular artery.
The vas deferens is the direct continuation of the tail of the epididymis. It runs upwards medial to the epididymis and so enters the spermatic cord. The blood supply of the vas is from the artery to the vas, a branch of the inferior vesical artery.
Blood supply, lymphatic drainage and cutaneous innervation of the scrotum
The anterior surface of the scrotal wall derives its blood supply from the superficial and deep external pudendal arteries bilaterally. Both arteries are early branches of the (common) femoral artery. They arise from the latter just below the level of the inguinal ligament, run medially and supply the anterior aspect of the scrotum of their side. The posterior aspect of the scrotal wall obtains its blood supply from the posterior scrotal arteries which are branches of the perineal artery, in turn a branch of the internal pudendal artery. Arteries in the anterior scrotal wall tend to run transversely, while those supplying the posterior aspect of the scrotal wall run longitudinally. Flaps can therefore be harvested from the well-vascularized scrotal skin and transferred to the urethra, penile shaft and the inguinal region.
Venous drainage from the wall of the scrotum is predominantly via the superficial and deep external pudendal veins, on each side, to the ipsilateral great saphenous vein. However, the midline of the scrotum drains medially and not laterally which is an important consideration when faced with conditions such as scrotal lymphedema.
Lymphatic drainage from the scrotal wall is to the ipsilateral superficial inguinal lymph nodes. Lymphatic drainage of the scrotal contents, however, is different. Lymphatics from the testis run within the spermatic cord and eventually drain to the para-aortic lymph nodes near the origin of the gonadal arteries (at approximately L2 vertebral level). Lymphatics from the epididymis drain principally to the ipsilateral internal iliac lymph nodes.
Cutaneous innervation of the anterior aspect of the scrotum is by the right and left ilioinguinal nerves (L1). Each nerve innervates the anterior third of the corresponding hemiscrotum. The genital branch of the genitofemoral nerve makes a minor contribution. The posterior scrotal skin is innervated by the scrotal branches of the perineal nerve (branch of the pudendal nerve) with an additional contribution from the perineal branch of the posterior femoral cutaneous nerve. The posterior scrotal skin corresponds to the S3 dermatome.
The dartos muscle in the scrotal wall is innervated by sympathetic fibers conveyed by the genital branch of the geni...