Topographical and Pathotopographical Medical Atlas of the Pelvis, Spine, and Limbs
Z. M. Seagal
- English
- ePUB (handyfreundlich)
- Über iOS und Android verfügbar
Topographical and Pathotopographical Medical Atlas of the Pelvis, Spine, and Limbs
Z. M. Seagal
Über dieses Buch
The fourth medical atlas in this new series on the human body and filled with detailed pictures, this atlas details the topographical and pathotopographical anatomy of the pelvis, spine, and limbs, a useful reference for medical professionals and students alike.
Written by an experienced and well-respected physician and professor, this new volume, building on the previous volume, Ultrasonic Topographical and Pathotopographical Anatomy, and its sequels, also available from Wiley-Scrivener, presents the ultrasonic topographical and pathotopographical anatomy of the pelvis, spine, and limbs, offering further detail into these important areas for use by medical professionals.
This series of atlases of topographic and pathotopographic human anatomy is a fundamental and practically important series designed for doctors of all specializations and students of medical schools. Here you can find almost everything that is connected with the topographic and pathotopographic human anatomy, including original graphs of logical structures of topographic anatomy and development of congenital abnormalities, topography of different areas in layers, pathotopography, computer and magnetic resonance imaging (MRI) of topographic and pathotopographic anatomy. Also you can find here new theoretical and practical sections of topographic anatomy developed by the author himself which are published for the first time. They are practically important for mastering the technique of operative interventions and denying possibility of iatrogenic complications during operations.
This important new volume will be valuable to physicians, junior physicians, medical residents, lecturers in medicine, and medical students alike, either as a textbook or as a reference. It is a must-have for any physician's library.
Häufig gestellte Fragen
Information
Part 1:
The Pelvis
Topographic Anatomy of the Pelvis
Individual, Gender and Age Differences:
- The individual features of the pelvis consist of different ratios of the longitudinal and transverse diameters of the pelvic ring. At one extreme type of variability, the longitudinal diameter is greater than the transverse one, the pelvis is “squeezed” from the sides, and the axes of the pelvic organs are often inclined to the sacrum. With a different type of variability, the longitudinal diameter is less than the transverse one, the pelvis is “compressed” in the anteroposterior direction, and the axes of the pelvic organs are inclined toward the pubic symphysis.
- The gender differences. The wings of the iliac bones in women are more horizontal, therefore in women the pelvis is wider and lower than that of men. The inferior branches of pubic bones in women are located at an obtuse angle and form a pubic arch (arcus pubis); in men they are located at an acute angle and form a subpubic angle (angulus subpubicus). The pelvic cavity in women has the shape of a curved cylinder; in men it has the shape of a curved cone. The incline of the pelvis (inclination pelvis) is the angle between the horizontal plane and the plane of the superior aperture of the pelvis. In women it’s 55–60°, in men – 50–55°.
- Age differences. By the time of birth, the pelvic consists of three parts, each of which has ossification centers. All three parts – iliac, ischial and pubic – are connected inter-layer cartilage in the area of the acetabulum. The iliac fossa is almost absent. By the age of seven, the size of the pelvic bone doubles, then the growth slows to 12 years. By the age of 13–18, parts of the pelvic bone coalesce, and their ossification ends. The synostosis of all elements of the hipbone is completed by the age of 25.
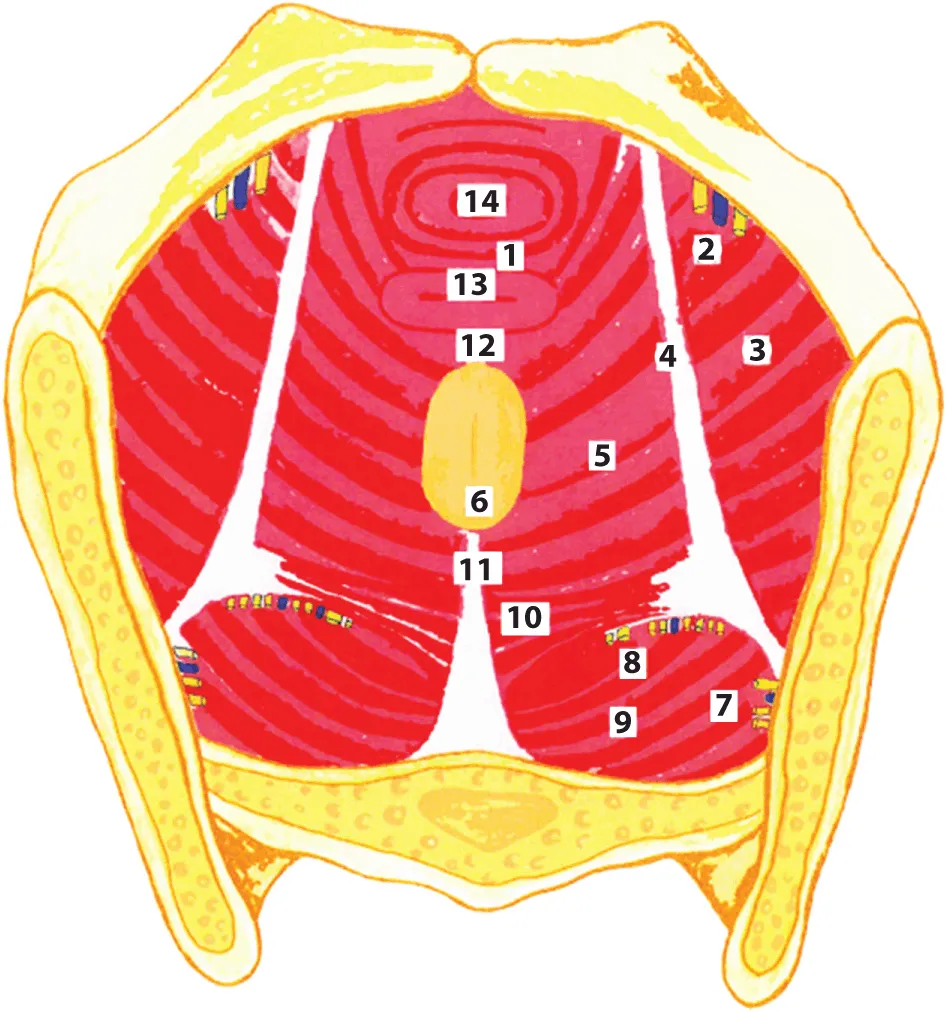
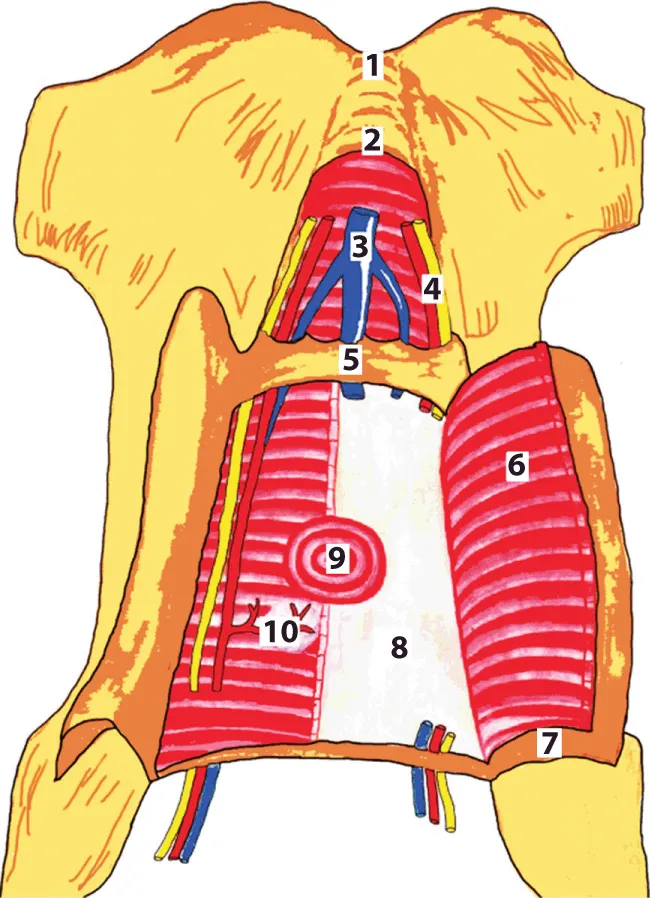
1 – diaphragma urogenitalis; 2 – nn. et vasa obturatorii; 3 – m. obturatorius internus; 4 – arcus tendineus m. levatoris ani; 5 – m. levator ani; 6 – anus; 7 – nn. et vasa glutei superiores; 8 – n. ischiadicus et fasc. gluteus inferior; 9 – m. piriformis; 10 – m. coccygeus; 11 – lig. anococcygeus; 12 – centrum tendineum perinei; 13 – vagina; 14 – urethra
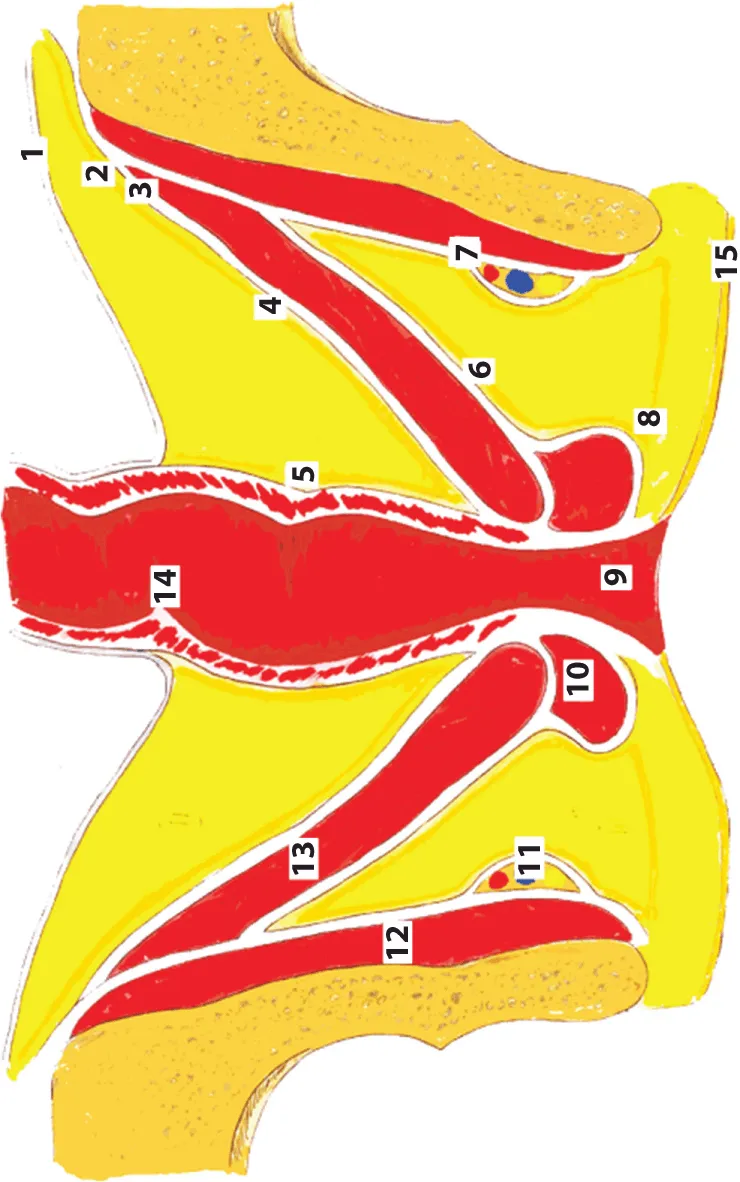
1 – peritoneum; 2 – fascia intraperitonealis; 3 – arcus tendneus; 4 – the parietal peritoneum; 5 – the visceral peritoneum; 6 – the deep perineal fascia; 7 – fascia m. obturatorii; 8 – the superficial perineal fascia; 9 – anus; 10 – m. sphincter ani externi; 11 – canalis pro vasa pudendi et n.; 12 – m. obduratorius internus; 13 – m. levator ani; 14 – rectum; 15 – derma perinei
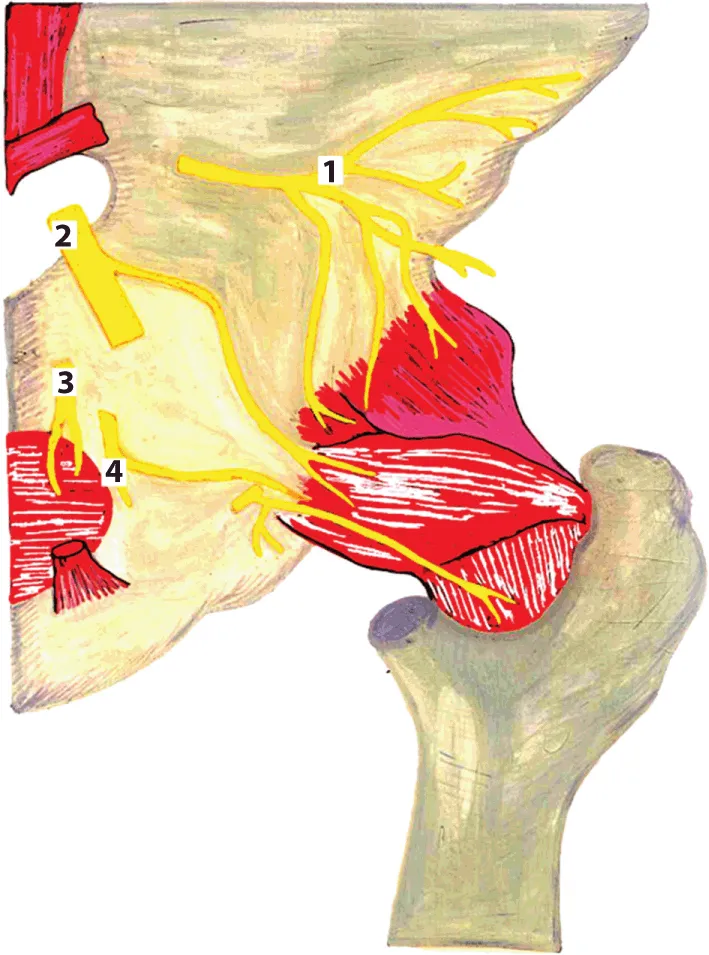
1 – n. gluteus superior; 2 – n. ischiadicus; 3 – n. pudendus; 4 – n. gluteus inferior
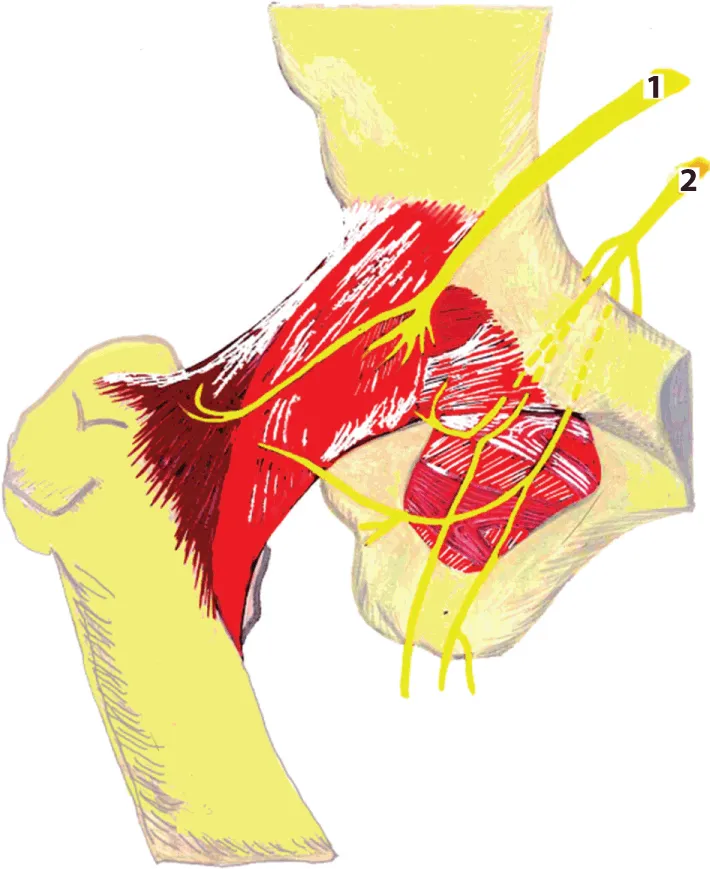
1 – n. femoralis; 2 – n. obturatorius
1 – symphisis ossium pubis; 2 – lig. arcuaturn pubis; 3 – v. penis; 4 – a. et n. penis; 5 – lig. transversum perinea; 6 – m. transversus perinei profundus; 7 – folium superficialis aponeurosis urogenitalis; 8 – folium profundum aponeurosis urogenitalis; 9 – urethra et m. sphincter urethrae; 10 – glandula bulbourethralis
Inhaltsverzeichnis
- Cover
- Title Page
- Copyright
- Introduction
- Part 1: The Pelvis
- Part 2: The Spine
- Part 3: The Limbs
- Conclusion
- About the Author
- End User License Agreement