eBook - ePub
Mood Disorders
Practical Issues in Diagnosis and Management
Ather Muneer
This is a test
- 212 páginas
- English
- ePUB (apto para móviles)
- Disponible en iOS y Android
eBook - ePub
Mood Disorders
Practical Issues in Diagnosis and Management
Ather Muneer
Detalles del libro
Vista previa del libro
Índice
Citas
Información del libro
Mood Disorders: Practical Issues in Diagnosis and Management provides cutting edge knowledge about the diagnosis and treatment of principal mood disorders, namely major depressive disorder and bipolar disorder. Covering diagnosis, differentiating features, and illness course and trajectories of principal mood disorders, Dr. Ather Muneer provides essential information in a succinct and practical manner, while highlighting significant new findings in the area. This book will help a broad range of mental health professionals better treat the millions ofpeople withmood disorders across the globe.
Preguntas frecuentes
¿Cómo cancelo mi suscripción?
¿Cómo descargo los libros?
Por el momento, todos nuestros libros ePub adaptables a dispositivos móviles se pueden descargar a través de la aplicación. La mayor parte de nuestros PDF también se puede descargar y ya estamos trabajando para que el resto también sea descargable. Obtén más información aquí.
¿En qué se diferencian los planes de precios?
Ambos planes te permiten acceder por completo a la biblioteca y a todas las funciones de Perlego. Las únicas diferencias son el precio y el período de suscripción: con el plan anual ahorrarás en torno a un 30 % en comparación con 12 meses de un plan mensual.
¿Qué es Perlego?
Somos un servicio de suscripción de libros de texto en línea que te permite acceder a toda una biblioteca en línea por menos de lo que cuesta un libro al mes. Con más de un millón de libros sobre más de 1000 categorías, ¡tenemos todo lo que necesitas! Obtén más información aquí.
¿Perlego ofrece la función de texto a voz?
Busca el símbolo de lectura en voz alta en tu próximo libro para ver si puedes escucharlo. La herramienta de lectura en voz alta lee el texto en voz alta por ti, resaltando el texto a medida que se lee. Puedes pausarla, acelerarla y ralentizarla. Obtén más información aquí.
¿Es Mood Disorders un PDF/ePUB en línea?
Sí, puedes acceder a Mood Disorders de Ather Muneer en formato PDF o ePUB, así como a otros libros populares de Medicine y Psychiatry & Mental Health. Tenemos más de un millón de libros disponibles en nuestro catálogo para que explores.
Información
1Major Depressive Disorder and Bipolar Disorder
Introduction
According to the Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-5) major mood disorders are classified into major depressive disorder (MDD) and bipolar disorder (BD). More than a century ago, the German psychiatrist Emil Kraepelin categorized major mental disorders into “manic depressive insanity” and “dementia praecox”. The former was re-conceptualized as a recurrent illness exemplified by repeated depressive and manic episodes while the latter was replaced by “schizophrenia”, a word coined by the Swiss psychologist Eugene Bleuler and typified as a non-affective psychosis epitomized by delusions, hallucinations, blunting of affect and loss of motivation.1 In the current rendition of DSM-5, MDD and BD are described under separate rubrics as these mood disorders are presently considered to have distinct etiology, pathogenesis, course and therapeutic connotations.
Major mood disorders are highly prevalent conditions affecting up to 20% of the general population.2 Individuals of both sexes are afflicted, onset is usually in teenage years or early adulthood and the disorders follow a relapsing and remitting course throughout life. All the current treatments are palliative rather than curative in nature, and while the modern psychopharmacological agents have improved safety and efficacy, these still impose a huge burden with respect to adverse effects. Consequently, compliance is low and relapse rate is high with resultant impairment in the biopsychosocial realms of functioning.3 Affective disorders are a leading cause of morbidity and mortality, since these are regarded as systemic ailments and are very often associated with such comorbid conditions as diabetes mellitus, cardiovascular diseases, autoimmune disorders and endocrine disturbances.4 The majority of people who commit suicide have an underlying mood disorder, and new data suggest that the incidence of this condition is on the rise across the world.5 Because of these reasons World Health Organization statistics show that mood disorders are an important source of disability and death globally.6 Therefore, in the light of such considerations it is crucial that physicians in general and mental health professionals in particular, have an adequate understanding of these very common psychiatric conditions.
Signs and Symptoms
Historical development in the nosology of mood disorders has led to their categorization into unipolar depression and BD. Essentially these are distinct conditions with different genetic underpinnings and disparate illness trajectory, progression and outcome. In essence, MDD is typified by recurrent depressive exacerbations without a lifetime history of hypomanic or manic episodes, whereas BD patients fluctuate between the opposite mood states of depression and mania.7
Major Depressive Episode
A major depressive episode (MDE) is signified by the presence of low mood and loss of pleasure in day-to-day activities, aptly termed anhedonia. The latter represents a distinct emotional tone in the patients, wherein they lose interest in the usual activities and no longer experience pleasure in things they previously found enjoyable. The cognitive process in MDE is exemplified by excessive guilt and self-blame, thoughts of helplessness and hopelessness and suicidal ideation. Disruption in the circadian rhythm is evident as sleep disturbance, with early morning wakening characterizing the more severe, melancholic form of MDD. There is usually decreased appetite and weight loss, but patients with “atypical depression” can have reverse vegetative disturbance with hypersomnia, increased food intake and weight gain. Subjects who have MDEs experience excessive mental and physical fatigue, loss of energy and tiredness and also complain of difficulty in concentration and indecisiveness. Further, they may show psychomotor retardation or agitation. Recurrent suicidal ideation and psychomotor agitation accompanying a low mood predisposes MDD patients to self-harm and attempted or completed suicide.8 While the duration criteria stipulate a minimum period of two weeks, in the usual scenario patients are symptomatic for months before they seek medical help. As can be construed from the abovementioned facts, an MDE is a serious ailment which can prove fatal if there is delay in diagnosis and treatment. The vast majority of patients with MDD follow a relapsing and remitting course, and while it is possible to have a single lifetime MDE, this is the exception rather than the rule.9
Manic Episode
A manic episode is the sine qua non of BD and patients typically present with elevated or expansive mood. They have raised self-esteem and express grandiose ideas, which in the case of psychotic mania can be of delusional intensity. Subjectively, patients experience racing thoughts and objectively this is manifested as pressure of speech and flight of ideas. They have boosted energy levels and show increase in goal-directed activities; coupled with this is a decreased need for sleep. In severe mania, the patient is on the go most of the time, has boundless energy and feels rested after only a few hours of sleep. These subjects exhibit overindulgence in pleasurable activities and become part of risky ventures with high potential for harmful social consequences. Some examples are buying sprees, sexual indiscretions, and alcohol and substance abuse. A manic patient requires urgent treatment and is often in need of psychiatric hospitalization. Whereas the duration criteria stipulate a period of disturbance spanning one week, if hospitalization is mandated then a manic episode can be diagnosed with any period of mood disturbance.10 The core symptoms of a hypomanic episode are essentially analogous to a manic episode, with the caveat that severe psychosocial disruption is not evident and emergency hospitalization is not needed.11 Only four days of mood disturbance is sufficient to diagnose a hypomanic episode and, while the disorder is subtle in presentation, it is often part of chronic affective instability in bipolar spectrum disorders.
Mixed States
Mood symptoms can manifest in numerous ways and typical presentations are seen in only a minority of patients. A common clinical occurrence is the presence of mixed affective states, which can afflict people with both MDD and BD. The current conceptualization of mixed states posits that symptoms of opposite mood polarity are attendant in patients with major mood disorders. It is estimated that up to 40% of bipolar patients may be afflicted in this manner, while concurrent presence of hypomanic or manic symptoms in MDD is being increasingly recognized.12 In essence, this implies that patients with manic or hypomanic episodes have coexisting depressive symptoms and vice versa. The clinical significance of mixed states is manifold. Firstly, the clinician should be cognizant of their occurrence and be on the lookout for the presence of mixed affective manifestations in patients with mood disorders. Secondly, it should be realized that repeated episodes of similar polarity occur, such that patients with mixed episodes tend to have the same exacerbations in the course of their illness. Thirdly, mixed episodes signify a more severe illness trajectory marked by treatment resistance, greater neuropsychiatric comorbidities and higher risk of suicide. Lastly, polypharmacy is the rule rather than the exception in the management of these cases and there is consequential patient noncompliance from medication adverse effects.13
Figure 1.1 is an illustrative rendition of the different mood states as envisaged in DSM-5. Table 1.1 recapitulates the main affective states as encountered in discrete mood episodes.
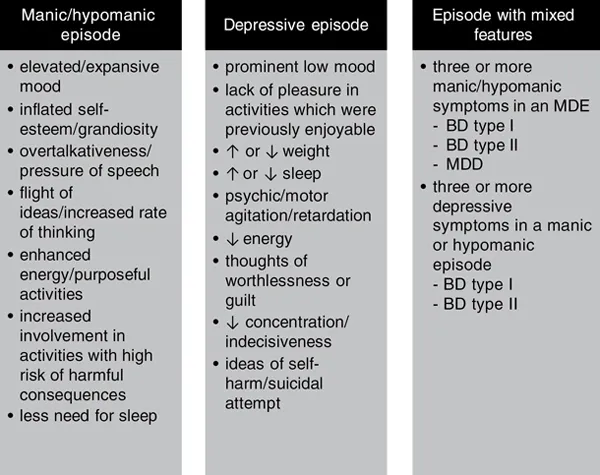
Figure 1.1Diagnostic criteria for manic, depressive and mixed states according to DSM-5
As opposed to previous editions, in DSM-5 the specifier “with mixed features” is used for manic, hypomanic or depressive episodes in bipolar spectrum and major depressive disorders. The term “mixed episode” employed in the setting of BD type I has been discontinued in DSM-5.
BD – bipolar disorder; MDD – major depressive disorder; MDE – major depressive episode
Table 1.1Diagnostic features of different affective states according to DSM-5
| Symptom domain | Hypo/manic episode | Depressive episode | Episode with mixed features |
| Subjective mood | Elated | Depressed | Varies |
| Hedonic tone | ↑involvement in pleasurable activities | Anhedonia | Mixture of both |
| Thought content | Grandiose | Worthlessness/guilt | Varies |
| Talk | ↑in rate, rhythm and volume | ↓in rate, rhythm and volume | Incongruent e.g. depressed mood with pressure of speech |
| Behavior | Risky behaviors | Suicidal acts | Contrasting e.g. elevated mood with suicidal ideation |
| Energy | ↑ | ↓ | ↑↓ |
| Sleep | ↓need for sleep | Early morning wakening | Severely disturbed |
| Thoughts | Racing thoughts | Difficulty in thinking/concentration | Incongruent e.g. depressed mood with racing thoughts |
| Appetite/weight | Disrupted meal schedule | ↓ | Severe disruption |
| Duration | Hypomania – 4 days; mania – 7 days | 14 days | Duration criteria no longer apply |
| Minimum criteria for mixed episode | Three depressive features in hypomanic or manic episode | Three manic features in a depressive episode | Mixed hypomania – BD type I or II Mixed mania – BD type I MDE with mixed features – BD type I or II/MDD |
| Functioning | Hypomania – impaired but does not require hospitalization Mania – severely impaired/may need hospitalization | Impaired according to degree – mild/moderate/severe | Varies according to diagnosis |
BD – bipolar disorder; MDD – major depressive disorder; MDE – major depressive episode
Diagnosis of Mood Diso...
Índice
- Cover
- Half Title
- Title Page
- Copyright Page
- Contents
- List of Figures
- List of Tables
- 1 Major Depressive Disorder and Bipolar Disorder
- 2 Major Mood Disorders: Differentiating Features
- 3 Comorbidity in Mood Disorders
- 4 The Role of Epigenetics
- 5 Neurobiology of Mood Disorders: The Circadian Connection
- 6 Pathogenesis of Mood Disorders: The Neuroinflammatory Hypothesis
- 7 Staging and Neuroprogression of Mood Disorders
- 8 The Management of Treatment-Resistant Depression: Monoamines and Beyond
- 9 Depressive Phase of Bipolar Disorder: Treatment Recommendations
- 10 Manic Phase of Bipolar Disorder: Treatment Recommendations
- 11 Non-Pharmacological Treatments for Mood Disorders
- Index
Estilos de citas para Mood Disorders
APA 6 Citation
Muneer, A. (2018). Mood Disorders (1st ed.). Taylor and Francis. Retrieved from https://www.perlego.com/book/1580270/mood-disorders-practical-issues-in-diagnosis-and-management-pdf (Original work published 2018)
Chicago Citation
Muneer, Ather. (2018) 2018. Mood Disorders. 1st ed. Taylor and Francis. https://www.perlego.com/book/1580270/mood-disorders-practical-issues-in-diagnosis-and-management-pdf.
Harvard Citation
Muneer, A. (2018) Mood Disorders. 1st edn. Taylor and Francis. Available at: https://www.perlego.com/book/1580270/mood-disorders-practical-issues-in-diagnosis-and-management-pdf (Accessed: 14 October 2022).
MLA 7 Citation
Muneer, Ather. Mood Disorders. 1st ed. Taylor and Francis, 2018. Web. 14 Oct. 2022.